Cold and Flu Medicines: A Complete, Easy-to-Understand Guide for Safe and Effective Relief
Introduction
Cold and flu medicines are among the most widely used healthcare products worldwide, especially during seasonal changes and winter months. Almost everyone experiences a cold or flu at least once a year, and many rely on cold and flu medications to reduce discomfort and continue daily activities. While these medicines do not cure viral infections, they play a vital role in relieving symptoms, improving comfort, and supporting recovery.
The common cold and influenza (flu) are caused by viruses, which means antibiotics are ineffective. Instead, cold and flu medicines are designed to target specific symptoms, such as fever, body aches, sore throat, nasal congestion, runny nose, and cough. Understanding how these medicines work helps people choose the most effective treatment while avoiding unnecessary risks.
Most cold and flu medicines are available over the counter (OTC), making them easy to access. However, misuse is common. Taking the wrong medicine, mixing products with the same ingredients, or exceeding recommended doses can lead to serious side effects. For example, some cold and flu medicines may increase blood pressure, cause drowsiness, or interact with existing medications.
Why Cold and Flu Medicines Are So Commonly Used
Cold and flu medicines are popular because they provide fast and targeted symptom relief. When symptoms disrupt sleep, work, or daily routines, these medicines help restore comfort and functionality.
Common reasons people use cold and flu medicines include:
- Relief from fever and body aches
- Reduction of nasal congestion and sinus pressure
- Control of cough and throat irritation
- Management of runny nose and sneezing
- Improved sleep with night-time cold and flu medicines
Health data shows that adults experience an average of 2–3 colds per year, while children may experience even more. Influenza affects millions annually and can be severe in older adults, pregnant women, and people with chronic conditions. This makes cold and flu medicines a key part of everyday symptom management.
Treating Symptoms vs Curing the Illness
A critical fact about cold and flu medicines is that they do not eliminate viruses. Their purpose is to relieve symptoms while the immune system fights the infection naturally.
“Cold and flu medicines manage symptoms, not the virus itself. Rest, hydration, and time are essential for recovery.”
This explains why symptoms may last several days even when taking medication. Using the right cold and flu medicines can make recovery more comfortable, but they work best when combined with proper rest, hydration, and nutrition.
Common Myths About Cold and Flu Medicines
There are many misunderstandings surrounding cold and flu treatment. Some of the most common myths include:
- “Stronger medicine means faster recovery” – Recovery depends on immune response, not medicine strength.
- “Antibiotics treat colds and flu” – Antibiotics do not work against viruses.
- “Taking more medicine works better” – Overdosing increases the risk of serious side effects.
- “Combination cold and flu medicines are always best” – Single-ingredient medicines are often safer.
Understanding these myths helps people use cold and flu medicines safely and effectively.
What Is the Difference Between a Cold and the Flu?
Understanding the difference between a common cold and influenza (flu) is essential when choosing the right cold and flu medicines. Although both illnesses affect the respiratory system and share similar symptoms, they differ significantly in severity, duration, and treatment approach. Using the wrong type of medicine can lead to poor symptom control or unnecessary side effects.
Many people mistake the flu for a severe cold, but influenza is usually much more intense and can lead to serious complications, especially in older adults, young children, and people with weak immune systems.
Cold vs Flu: Key Differences Explained
The table below highlights the most important differences between a cold and the flu and how they impact the use of cold and flu medicines:
| Feature | Common Cold | Influenza (Flu) |
|---|---|---|
| Onset of symptoms | Gradual | Sudden |
| Fever | Rare or mild | High (38–40°C) |
| Body aches | Mild | Severe |
| Fatigue | Mild | Extreme |
| Cough | Mild to moderate | Severe, dry cough |
| Headache | Rare | Common |
| Duration | 5–7 days | 7–14 days or longer |
| Complications | Rare | Pneumonia, hospitalization |
This distinction matters because cold and flu medicines are symptom-based, and flu symptoms often require stronger or more targeted treatment strategies.
Symptoms of the Common Cold
The common cold is usually mild and manageable with basic cold and flu medications. Typical cold symptoms include:
- Runny or stuffy nose
- Sneezing
- Mild sore throat
- Mild cough
- Slight fatigue
- Low or no fever
Cold symptoms often improve within a few days, and most people can manage them with single-ingredient cold medicines, rest, and hydration.
Symptoms of Influenza (Flu)
The flu tends to hit suddenly and feels much more intense than a cold. Common flu symptoms include:
- High fever and chills
- Severe muscle and body aches
- Intense fatigue and weakness
- Dry, persistent cough
- Headache
- Chest discomfort
Because flu symptoms are stronger, people often rely on multi-symptom cold and flu medicines to manage pain, fever, and congestion simultaneously.
Severity Comparison: Why the Difference Matters
The flu can cause serious health complications, including bronchitis, pneumonia, and worsening of chronic conditions like asthma or heart disease. This is why people with flu symptoms may need more than standard cold and flu medicines, especially if symptoms worsen or last longer than expected.
“If symptoms are severe, sudden, or include high fever and extreme fatigue, flu—not a cold—is more likely.”
Recognizing severity helps users decide when OTC cold and flu medicines are sufficient and when medical care is necessary.
Duration of Illness and Medicine Choice
- Colds usually improve within a week and respond well to mild cold and flu medicines.
- Flu symptoms can last two weeks or more and may require stronger symptom relief or prescription antiviral treatment.
Choosing cold and flu medicines based on illness duration prevents unnecessary medication use and reduces health risks.
How Diagnosis Affects Cold and Flu Medicines
Correct identification of symptoms ensures safer treatment:
- Cold symptoms → nasal sprays, antihistamines, mild pain relievers
- Flu symptoms → fever reducers, pain relievers, rest, hydration
- Severe or persistent symptoms → medical consultation
Using targeted cold and flu medicines improves comfort while allowing the immune system to do its job effectively.
How Cold and Flu Medicines Work
To use cold and flu medicines safely and effectively, it is important to understand how they actually work inside the body. Many people assume these medicines cure colds or flu, but in reality, they are designed to manage symptoms, not eliminate the virus. This distinction helps set realistic expectations and prevents misuse.
Cold and flu viruses enter the body through the nose, mouth, or eyes and begin multiplying in the respiratory tract. The immune system responds by releasing chemicals that cause inflammation, fever, mucus production, and body aches. These reactions are part of the body’s defense system—but they are also responsible for most of the uncomfortable symptoms people experience.
Do Cold and Flu Medicines Cure Illness?
The simple answer is no. Cold and flu medicines do not kill viruses or shorten the infection in most cases. Instead, they reduce symptom intensity, making it easier for people to rest, sleep, and recover.
“Cold and flu medicines don’t fight the virus—they help you feel better while your immune system does.”
This is why rest, hydration, and proper nutrition remain just as important as medication.
How Different Cold and Flu Medicines Target Symptoms
Each category of cold and flu medicine works in a specific way:
- Pain relievers and fever reducers lower body temperature and ease muscle aches.
- Decongestants shrink swollen nasal blood vessels, improving airflow.
- Antihistamines reduce sneezing and runny nose by blocking histamine release.
- Cough suppressants calm the cough reflex.
- Expectorants loosen mucus, making coughs more productive.
By targeting specific symptoms, cold and flu medicines allow the body to heal with less discomfort.
The Role of the Immune System in Recovery
Even when using cold and flu medicines, the immune system remains the primary defense against infection. Fever, for example, helps slow viral replication, while mucus traps and removes pathogens.
This is why experts recommend not suppressing every symptom aggressively unless necessary. For example:
- Mild fever may not require treatment
- Mild congestion can resolve naturally
- Overuse of nasal sprays can worsen congestion
Understanding this balance helps people choose the right cold and flu medicines, not just more medicine.
Why Symptom-Based Treatment Works Best
Treating only the symptoms you have is safer and more effective than using multi-symptom products unnecessarily.
Example:
- If you only have a headache and fever → use a pain reliever
- If you have congestion only → use a decongestant
- If you have a cough with mucus → use an expectorant
This approach reduces side effects and lowers the risk of ingredient overlap or overdose.
Cold and Flu Medicines vs Antiviral Medications
It is important to distinguish between cold and flu medicines and antiviral drugs:
| Type | Purpose | Example |
|---|---|---|
| Cold and flu medicines | Symptom relief | Paracetamol, antihistamines |
| Antiviral medicines | Reduce flu severity | Oseltamivir |
Antivirals are prescription medicines used only in certain flu cases and must be taken early to be effective.
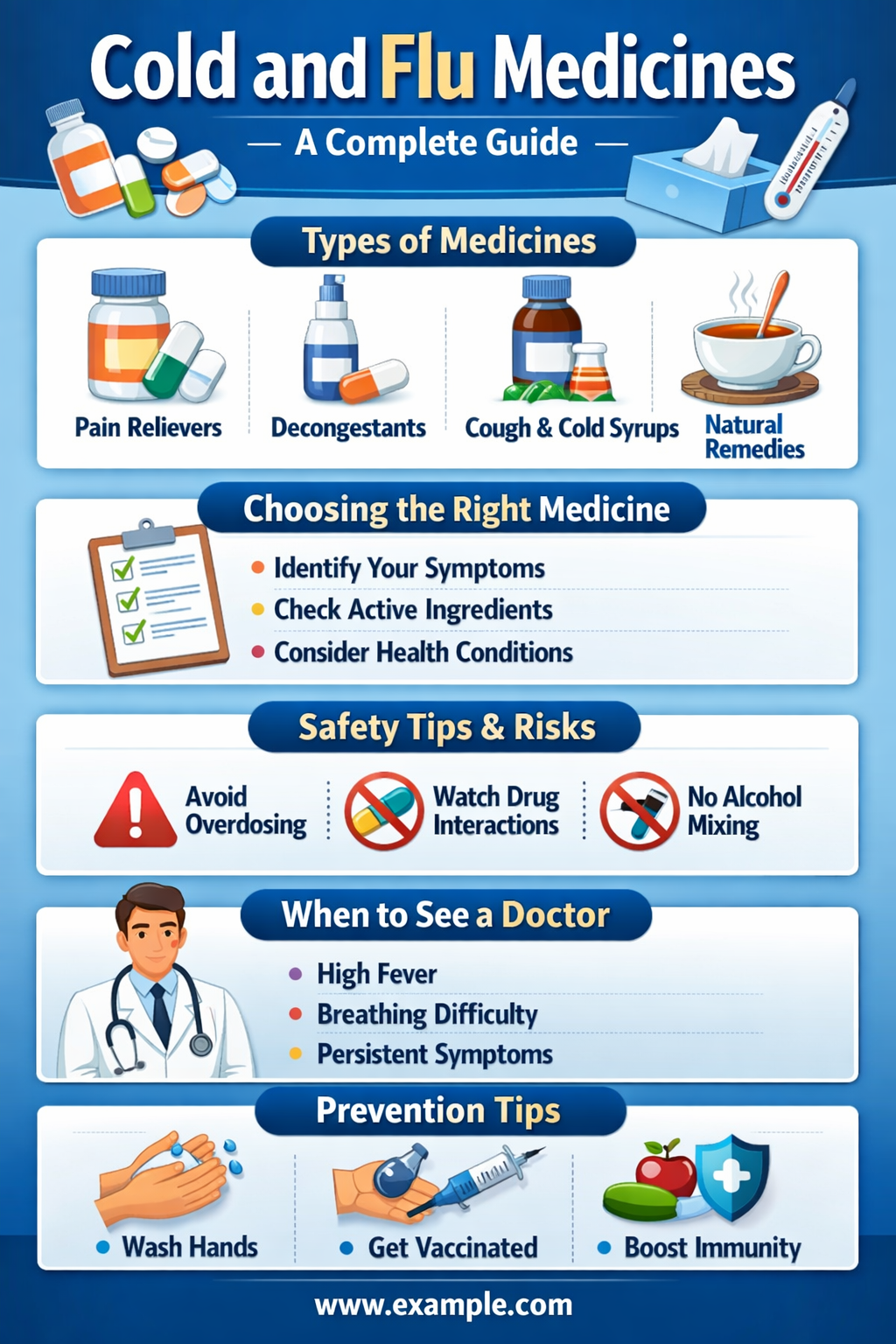
Types of Cold and Flu Medicines
There are many different types of cold and flu medicines, and each one is designed to relieve specific symptoms. Understanding these categories helps people avoid unnecessary medications and choose the safest, most effective option for their condition. Instead of using a “one-size-fits-all” product, symptom-based selection leads to better relief and fewer side effects.
Most over-the-counter cold and flu medicines fall into five main categories: pain relievers, decongestants, antihistamines, cough medicines, and combination products.
1. Pain Relievers and Fever Reducers
Pain relievers and fever reducers are among the most commonly used cold and flu medicines. They help reduce fever, headaches, sore throat pain, and body aches, which are common in both colds and flu.
Common active ingredients include:
- Acetaminophen (Paracetamol) – Gentle on the stomach and widely used
- Ibuprofen – Reduces inflammation and pain
- Aspirin – Effective but not recommended for children
How they work:
These medicines act on the brain and nervous system to lower fever and block pain signals. They do not treat congestion or cough but are highly effective for flu-related body pain.
Safety tips:
- Do not exceed daily dosage limits
- Avoid mixing multiple products containing acetaminophen
- Children should not take aspirin due to the risk of Reye’s syndrome
2. Decongestants for Cold and Flu Relief
Decongestants are cold and flu medicines designed to relieve stuffy nose and sinus pressure. They work by narrowing swollen blood vessels in the nasal passages, allowing easier breathing.
Types of decongestants:
- Oral decongestants (tablets or syrups)
- Nasal sprays
Benefits:
- Fast relief from nasal blockage
- Improved breathing and sleep
Risks and precautions:
- Can raise blood pressure and heart rate
- Nasal sprays should not be used for more than 3–5 days
- Not recommended for people with heart disease or hypertension
3. Antihistamines in Cold and Flu Medicines
Antihistamines are commonly included in cold and flu medicines to reduce runny nose, sneezing, and watery eyes.
Two main types:
- First-generation antihistamines – Cause drowsiness
- Second-generation antihistamines – Less sedating
When they help most:
- Early cold symptoms
- Night-time cold and flu medicines for sleep
Common side effects:
- Drowsiness
- Dry mouth
- Blurred vision
4. Cough Suppressants and Expectorants
Cough is one of the most persistent symptoms of cold and flu. Different cold and flu medicines are used depending on the type of cough.
| Cough Type | Best Medicine |
|---|---|
| Dry cough | Cough suppressants |
| Wet cough | Expectorants |
Key ingredients:
- Dextromethorphan – Suppresses cough reflex
- Guaifenesin – Loosens mucus
Using the wrong cough medicine may worsen symptoms, so identifying the cough type is important.
5. Combination Cold and Flu Medicines
Combination cold and flu medicines contain multiple active ingredients in one product. These are popular for convenience but require careful use.
Advantages:
- Treat multiple symptoms at once
- Easy to use
Disadvantages:
- Higher risk of ingredient overlap
- Increased side effects
- Unnecessary ingredients for some users
Quick Comparison of Cold and Flu Medicine Types
| Category | Treats | Key Caution |
|---|---|---|
| Pain relievers | Fever, aches | Overdose risk |
| Decongestants | Nasal blockage | Blood pressure |
| Antihistamines | Runny nose | Drowsiness |
| Cough medicines | Cough | Wrong type misuse |
| Combination products | Multiple symptoms | Ingredient overlap |
Best Cold and Flu Medicines for Common Symptoms
Choosing the right cold and flu medicines depends on the specific symptoms you are experiencing. Treating only the symptoms you have—rather than using multi-symptom products unnecessarily—can improve effectiveness and reduce side effects. Below is a symptom-based guide to selecting the most appropriate cold and flu medications.
Best Cold and Flu Medicines for Fever and Body Aches
Fever and body pain are especially common with influenza but can also occur with severe colds. Pain relievers and fever reducers are the first-line cold and flu medicines for these symptoms.
Most effective options include:
- Acetaminophen (paracetamol) – Safe for most people when used correctly
- Ibuprofen – Helps with inflammation and muscle pain
- Always follow dosage instructions
- Avoid taking two medicines with the same active ingredient
- Stay hydrated to support fever reduction
Best Cold and Flu Medicines for Stuffy Nose and Sinus Pressure
Nasal congestion can make breathing and sleeping difficult. Decongestants are commonly used cold and flu medicines for this symptom.
Effective choices include:
- Oral decongestants for all-day relief
- Nasal sprays for fast, short-term relief
Important safety notes:
- Limit nasal spray use to 3–5 days
- People with high blood pressure should avoid many decongestants
- Use saline sprays as a safer alternative when possible
Best Cold and Flu Medicines for Sore Throat
A sore throat is often caused by inflammation and post-nasal drip. Cold and flu medicines that reduce pain and swelling can help.
Helpful options include:
- Pain relievers (paracetamol or ibuprofen)
- Throat lozenges and sprays
- Warm fluids and saltwater gargles
Best Cold and Flu Medicines for Cough
Cough treatment depends on the type of cough.
For dry coughs:
- Cough suppressants help reduce irritation
For productive (wet) coughs:
- Expectorants loosen mucus
Avoid this mistake:
Using cough suppressants for wet coughs can trap mucus and worsen congestion.
Best Night-Time Cold and Flu Medicines
Night-time cold and flu medicines are designed to relieve symptoms that disrupt sleep.
Common features include:
- Antihistamines for runny nose
- Pain relievers for aches
- Mild sedative effects for sleep
Quick Symptom-to-Medicine Guide
| Symptom | Recommended Cold and Flu Medicine |
|---|---|
| Fever | Paracetamol, ibuprofen |
| Body aches | Pain relievers |
| Stuffy nose | Decongestants |
| Runny nose | Antihistamines |
| Dry cough | Cough suppressants |
| Wet cough | Expectorants |
Cold and Flu Medicines for Children
Using cold and flu medicines for children requires extra caution. Children are more sensitive to medications, and improper use can lead to serious side effects. In recent years, health authorities have issued strong warnings about the misuse of cold and flu medicines in young children, making it essential for parents and caregivers to understand what is safe and what is not.
Are Cold and Flu Medicines Safe for Kids?
Not all cold and flu medicines are safe for children. Many combination products are not recommended for children under 6 years of age, and some should be avoided even up to age 12.
Key reasons for caution include:
- Higher risk of overdose
- Increased sensitivity to side effects
- Difficulty measuring correct doses
- Presence of multiple active ingredients
Fact: Leading health organizations advise against using multi-symptom cold and flu medicines in young children due to safety concerns.
Age-Based Guidelines for Cold and Flu Medicines
| Age Group | Recommendation |
|---|---|
| Under 2 years | Avoid cold and flu medicines |
| 2–6 years | Use only if advised by a doctor |
| 6–12 years | Limited options with proper dosing |
| 12+ years | Many adult medicines may be used carefully |
Always check age labels and dosing instructions before giving any cold and flu medicine to a child.
Safer Options for Children’s Cold and Flu Symptoms
For children, symptom relief should focus on non-drug and single-ingredient treatments.
Safer choices include:
- Paracetamol for fever and pain
- Saline nasal drops for congestion
- Honey (for children over 1 year) to soothe cough
- Warm fluids and rest
Important: Never give aspirin to children due to the risk of Reye’s syndrome.
Why Combination Cold and Flu Medicines Are Risky for Kids
Combination cold and flu medicines often contain:
- Pain relievers
- Decongestants
- Antihistamines
- Cough suppressants
This increases the risk of ingredient overlap and overdose, especially if parents also give additional medicine separately.
Signs a Child Needs Medical Attention
Parents should seek medical care if a child has:
- High or persistent fever
- Difficulty breathing
- Severe cough or wheezing
- Symptoms lasting more than 7–10 days
- Signs of dehydration
Key Safety Tips for Parents
- Use proper measuring devices
- Never exceed recommended doses
- Avoid using adult cold and flu medicines
- Store medicines out of children’s reach
Using cold and flu medicines responsibly helps protect children while allowing their immune systems to recover naturally.
Prescription vs Over-the-Counter Cold and Flu Medicines
When it comes to cold and flu medicines, most people rely on over-the-counter (OTC) options, but there are situations where prescription medications may be necessary. Understanding the differences between OTC and prescription medicines helps users choose the safest and most effective treatment.
Over-the-Counter Cold and Flu Medicines
OTC medicines are widely available and can be purchased without a prescription. They are designed to relieve specific symptoms, including:
- Fever and body aches (pain relievers like paracetamol or ibuprofen)
- Runny nose and sneezing (antihistamines)
- Nasal congestion (decongestants)
- Cough (suppressants or expectorants)
Advantages of OTC medicines:
- Easy access
- Generally safe when used as directed
- Variety of single-ingredient and combination options
Limitations:
- Do not treat the underlying viral infection
- Multi-symptom products may increase risk of side effects
- Not suitable for children under certain ages or adults with specific health conditions
Prescription Cold and Flu Medicines
Prescription medications are usually recommended in special cases, particularly for influenza. They can help reduce symptom severity, shorten illness duration, or prevent complications. Examples include:
- Antiviral medications (e.g., oseltamivir, zanamivir) – Used for confirmed influenza cases, especially if started within 48 hours of symptom onset
- Stronger cough suppressants or combination products – Sometimes prescribed for persistent or severe symptoms
When prescription medicine is necessary:
- High-risk patients (elderly, pregnant women, or people with chronic illnesses)
- Severe flu symptoms (high fever, extreme fatigue, chest discomfort)
- Symptoms that do not improve with OTC cold and flu medicines
Note: Antibiotics are not effective for viral infections like colds or flu. They are only prescribed if a bacterial complication develops (e.g., sinus infection or pneumonia).
Key Differences Between OTC and Prescription Cold and Flu Medicines
| Feature | OTC Medicines | Prescription Medicines |
|---|---|---|
| Purpose | Symptom relief | Symptom relief + antiviral effects |
| Access | No prescription required | Prescription needed |
| Safety | Generally safe with label instructions | Must be monitored by a healthcare provider |
| Example | Paracetamol, decongestants | Oseltamivir, prescription-strength cough syrups |
Choosing the Right Option
For most healthy adults, OTC cold and flu medicines are sufficient to manage symptoms. Prescription medications are reserved for high-risk cases, confirmed flu, or severe symptoms. Always consult a healthcare provider if you are unsure about which medicine is appropriate.
Natural and Home Remedies vs Cold and Flu Medicines
Many people seek natural or home remedies to relieve cold and flu symptoms, either alone or alongside cold and flu medicines. While these remedies do not cure viral infections, they can support recovery, reduce discomfort, and complement medication safely.
Do Natural Remedies Work for Cold and Flu?
Natural remedies target symptoms rather than the virus itself. They can help:
- Reduce congestion
- Soothe sore throat
- Calm coughs
- Support hydration and immunity
Examples of effective remedies include:
- Herbal teas
- Chamomile, ginger, and peppermint teas can soothe a sore throat and ease congestion
- Warm liquids also promote hydration
- Honey
- Effective for reducing nighttime cough in children over 1 year and adults
- Has mild antimicrobial properties
- Steam inhalation or humidifiers
- Helps loosen mucus and reduce nasal irritation
- Moist air can improve breathing and comfort
- Vitamin C and Zinc
- May shorten duration of cold symptoms if taken early
- Supports immune system function
- Rest and hydration
- Essential for immune function and recovery
- Helps the body fight the infection naturally
How to Combine Natural Remedies with Cold and Flu Medicines
- Use natural remedies for comfort and supportive care
- Take cold and flu medicines only for symptom relief that interferes with daily life
- Avoid overloading the body with multiple treatments at once
Example:
A person with a mild cough can drink herbal tea and use honey, while someone with high fever may combine these remedies with paracetamol for fever and pain relief.
Benefits of Natural Remedies
- Low risk of side effects
- Cost-effective
- Often improves comfort and sleep
- Can be used safely in children and elderly when appropriate
Limitations
- Do not shorten the duration of infection significantly
- Cannot replace medicines for severe symptoms
- May interact with certain medications (e.g., herbal supplements affecting blood pressure or anticoagulants)
How to Choose the Right Cold and Flu Medicine
Selecting the right cold and flu medicine can feel overwhelming due to the wide variety of options available. Making the right choice ensures effective symptom relief, reduces side effects, and avoids unnecessary medication. The key is to base your selection on your specific symptoms, health conditions, and age.
Step 1: Identify Your Symptoms
Before picking any medicine, list the symptoms you want to treat. Common cold and flu symptoms include:
- Fever and body aches
- Nasal congestion or runny nose
- Sore throat
- Cough (dry or productive)
- Sneezing
- Fatigue and headache
Step 2: Check the Active Ingredients
Look for the active ingredients on the label:
- Paracetamol/Acetaminophen – Fever and body aches
- Ibuprofen – Pain and inflammation
- Pseudoephedrine or Phenylephrine – Nasal congestion
- Dextromethorphan – Dry cough
- Guaifenesin – Wet cough or mucus
- Antihistamines (diphenhydramine, loratadine) – Runny nose, sneezing
Avoid doubling up: Taking two products with the same active ingredient can cause overdose and serious side effects.
Step 3: Consider Your Health Conditions
Certain medicines may not be safe depending on your health:
- High blood pressure → avoid many decongestants
- Heart disease → avoid stimulant-based nasal sprays
- Kidney or liver problems → use pain relievers cautiously
- Pregnancy → check with a healthcare provider before taking any cold and flu medicine
Step 4: Consider Age and Weight
- Children: Use pediatric formulations and proper dosing devices
- Adults: Follow label instructions and monitor for side effects
- Elderly: Start with the lowest effective dose; watch for drowsiness and drug interactions
Step 5: Choose Day or Night Formulas
Some cold and flu medicines are designed for daytime use, minimizing drowsiness, while others are night-time formulas with mild sedatives to improve sleep. Select based on your daily routine and sleep needs.
Step 6: Avoid Unnecessary Combination Products
Combination products may contain multiple ingredients you don’t need. For instance:
- If you only have nasal congestion → single-ingredient decongestant may be safer
- If you only have a cough → avoid multi-symptom products with pain relievers or antihistamines
Rule of thumb: Use symptom-specific medicines whenever possible to reduce risk of side effects.
Step 7: Consult a Pharmacist or Doctor if Unsure
- If symptoms persist beyond 7–10 days
- If you have multiple chronic conditions
- If you are taking other medications
- If you are treating children or elderly individuals
A healthcare professional can recommend the safest and most effective cold and flu medicine.
Side Effects and Risks of Cold and Flu Medicines
While cold and flu medicines are generally safe when used correctly, they can cause side effects and health risks if misused. Understanding these potential issues helps users take medicines safely and avoid complications.
Common Side Effects
Each type of cold and flu medicine can cause different side effects:
- Pain relievers (paracetamol, ibuprofen): nausea, stomach upset, liver or kidney damage with overdose
- Decongestants: increased blood pressure, rapid heartbeat, insomnia
- Antihistamines: drowsiness, dry mouth, blurred vision, dizziness
- Cough suppressants: drowsiness, nausea, confusion in elderly patients
- Combination medicines: higher risk of multiple side effects due to multiple ingredients
Even mild side effects can interfere with daily activities, which is why taking the lowest effective dose is recommended.
Serious Risks to Watch For
Overuse or misuse of cold and flu medicines can lead to serious health problems:
- Paracetamol overdose – Can cause life-threatening liver damage
- Excess decongestants – Can trigger heart attack or stroke in high-risk individuals
- Combination overdose – Taking multiple products with the same active ingredient can be dangerous
- Drug interactions – Cold and flu medicines can interact with medications for blood pressure, heart disease, diabetes, and anticoagulants
Mixing Cold and Flu Medicines With Other Drugs
Always check labels and avoid combining:
- Multiple products containing acetaminophen or ibuprofen
- Decongestants with stimulant medications
- Cough suppressants with certain antidepressants
Alcohol and Cold and Flu Medicines
Some cold and flu medicines, particularly night-time formulations with antihistamines or sedatives, can interact with alcohol:
- Increased drowsiness
- Slower reaction times
- Risk of accidents
It’s best to avoid alcohol while taking cold and flu medicines that cause sedation.
Key Safety Guidelines
- Read the medicine label carefully
- Measure doses accurately
- Follow recommended frequency and duration
- Avoid unnecessary multi-symptom products
- Consult a healthcare provider if symptoms worsen or persist
Common Mistakes People Make with Cold and Flu Medicines
Even though cold and flu medicines are widely used, many people make mistakes that reduce effectiveness or create health risks. Avoiding these errors ensures safe and efficient symptom relief.
1. Taking Multiple Products With the Same Ingredient
One of the most common mistakes is accidentally doubling up on active ingredients. For example:
- Using a combination cold medicine containing paracetamol and taking a separate paracetamol tablet
- Taking multiple cough syrups with overlapping ingredients
Risk: Overdose, liver damage, or other serious side effects
2. Overusing Nasal Sprays
Decongestant nasal sprays provide fast relief, but overuse can cause rebound congestion, making symptoms worse.
- Limit use to 3–5 days
- Consider saline sprays for safer long-term relief
3. Ignoring Dosage Instructions
Some people take cold and flu medicines more frequently or in higher doses than recommended, hoping for faster relief.
Risks:
- Liver or kidney damage (with acetaminophen or NSAIDs)
- Heart complications (with decongestants)
4. Using Antibiotics for Viral Infections
Many people mistakenly believe antibiotics will treat colds or flu.
Fact: Colds and flu are caused by viruses, not bacteria. Antibiotics do not help and can lead to:
- Antibiotic resistance
- Unnecessary side effects
5. Taking Cold and Flu Medicines When Not Needed
- Using multi-symptom products when you have only one mild symptom
- Taking medicines too early or too late in illness
6. Mixing Medications With Alcohol
- Night-time cold and flu medicines often contain sedating antihistamines
- Alcohol can increase drowsiness, slow reaction times, and create safety risks
Rule: Avoid alcohol while using cold and flu medicines that cause drowsiness.
Summary of Common Mistakes
| Mistake | Risk | How to Avoid |
|---|---|---|
| Doubling up ingredients | Overdose | Check labels carefully |
| Overusing nasal sprays | Rebound congestion | Limit to 3–5 days |
| Ignoring dosage | Liver/kidney issues | Follow instructions |
| Using antibiotics | Ineffective | Only use for bacterial infections |
| Taking unnecessary meds | Side effects | Treat only symptoms |
| Mixing with alcohol | Increased sedation | Avoid alcohol |
Avoiding these mistakes improves recovery and reduces potential harm from cold and flu medicines.
When Cold and Flu Medicines Are Not Enough
While cold and flu medicines are effective for managing most symptoms, there are situations where medical attention is necessary. Recognizing the warning signs can prevent complications and ensure proper treatment.
When to See a Doctor
Seek professional help if you experience any of the following:
- Symptoms Lasting Too Long
- Colds usually resolve within 5–7 days
- Flu symptoms typically improve within 7–14 days
- Persistent fever, congestion, or cough beyond these timeframes may indicate complications
- High Fever
- Fever above 39°C (102°F) or lasting more than 3 days warrants medical evaluation
- Could indicate bacterial infection or severe flu
- Difficulty Breathing or Chest Pain
- Shortness of breath, wheezing, or chest discomfort may signal pneumonia or another serious respiratory condition
- Severe Dehydration or Weakness
- Signs include very little urination, dizziness, or extreme fatigue
- Especially concerning for children and elderly adults
- Underlying Health Conditions
- People with asthma, diabetes, heart disease, or weakened immune systems should consult a doctor if cold or flu symptoms appear
Why Cold and Flu Medicines May Not Be Enough
- They only relieve symptoms—they do not treat the underlying infection
- Some infections require prescription antivirals (for flu) or antibiotics (if bacterial complications develop)
- Severe symptoms may indicate complications that require medical monitoring
Preventing Complications
Even while using cold and flu medicines, these steps help reduce risks:
- Rest and sleep adequately
- Stay hydrated
- Monitor symptom progression daily
- Avoid self-medicating if symptoms worsen or new symptoms appear
Preventing Cold and Flu: Reducing the Need for Medicines
The best way to manage colds and flu is prevention. Reducing the likelihood of getting sick not only minimizes the need for cold and flu medicines but also helps protect overall health.
1. Practice Good Hand Hygiene
- Wash hands frequently with soap and water for at least 20 seconds
- Use alcohol-based hand sanitizer when soap is unavailable
- Avoid touching your face, especially the nose, mouth, and eyes, to prevent viral entry
Fact: Studies show proper hand hygiene can reduce respiratory infections by up to 21%.
2. Get Vaccinated
- Annual flu vaccine helps prevent influenza or reduce its severity
- Vaccination is especially important for children, elderly adults, pregnant women, and people with chronic illnesses
3. Strengthen the Immune System
Healthy lifestyle choices support immune function and reduce the severity of infections:
- Balanced diet rich in fruits, vegetables, and protein
- Regular physical activity
- Adequate sleep (7–9 hours for adults)
- Stress management through mindfulness or relaxation techniques
4. Avoid Close Contact During Peak Seasons
- Stay away from people who are sick when possible
- Wear masks in crowded or high-risk areas during flu season
- Maintain good ventilation indoors
5. Stay Hydrated and Support Respiratory Health
- Drink plenty of fluids to keep mucous membranes moist
- Use humidifiers in dry environments to prevent nasal irritation
- Gargle with salt water to reduce throat irritation
Frequently Asked Questions About Cold and Flu Medicines
Here are some of the most common questions people have about cold and flu medicines, answered in a simple, clear, and practical way.
1. Can cold and flu medicines cure the illness?
No. Cold and flu medicines do not cure the viral infection. They only relieve symptoms like fever, congestion, cough, and body aches, allowing the body to recover more comfortably.
2. Can I take multiple cold and flu medicines at the same time?
You can, but only if the active ingredients do not overlap. Taking multiple medicines with the same ingredient can cause overdose and serious side effects. Always read labels carefully.
3. Are cold and flu medicines safe for children?
Many cold and flu medicines are not recommended for children under 6 years old. Parents should use pediatric formulations and follow dosage instructions closely. Honey can be used for coughs in children over 1 year.
4. Can I use antibiotics for colds or flu?
No. Antibiotics do not work against viruses like the common cold or influenza. They are only used if a bacterial infection develops as a complication.
5. What are the best medicines for a stuffy nose?
Decongestants—oral or nasal sprays—are most effective. Saline sprays are safer for long-term use, and nasal sprays should not be used for more than 3–5 days to avoid rebound congestion.
6. How do I know if I need a doctor instead of OTC medicine?
Seek medical attention if you experience:
- High or persistent fever
- Difficulty breathing or chest pain
- Severe dehydration
- Symptoms lasting longer than 7–10 days
- High-risk conditions (e.g., elderly, pregnant, chronic illnesses)
7. Can natural remedies replace cold and flu medicines?
Natural remedies like herbal teas, honey, vitamin C, and steam inhalation support recovery but do not replace medicines for moderate to severe symptoms. They work best alongside symptom-targeted medications.
8. Is it safe to drink alcohol while taking cold and flu medicines?
Alcohol can increase drowsiness and side effects, especially with night-time formulas or antihistamines. It’s best to avoid alcohol while taking these medications.
9. Can cold and flu medicines shorten the duration of illness?
No. They relieve symptoms but do not significantly shorten the course of a viral infection. Recovery primarily depends on your immune system.
10. How do I choose the right cold and flu medicine?
- Identify your symptoms
- Check active ingredients
- Consider age, health conditions, and potential interactions
- Avoid unnecessary combination products
- Consult a pharmacist or doctor if unsure
Conclusion: Safe and Effective Use of Cold and Flu Medicines
Cold and flu medicines are essential tools for managing the discomfort of viral respiratory infections. While they cannot cure colds or flu, they provide symptom relief that helps people rest, recover, and maintain daily activities. Understanding how these medicines work, selecting the right product, and using them safely ensures the best possible outcome.