What is Respiratory Acidosis?
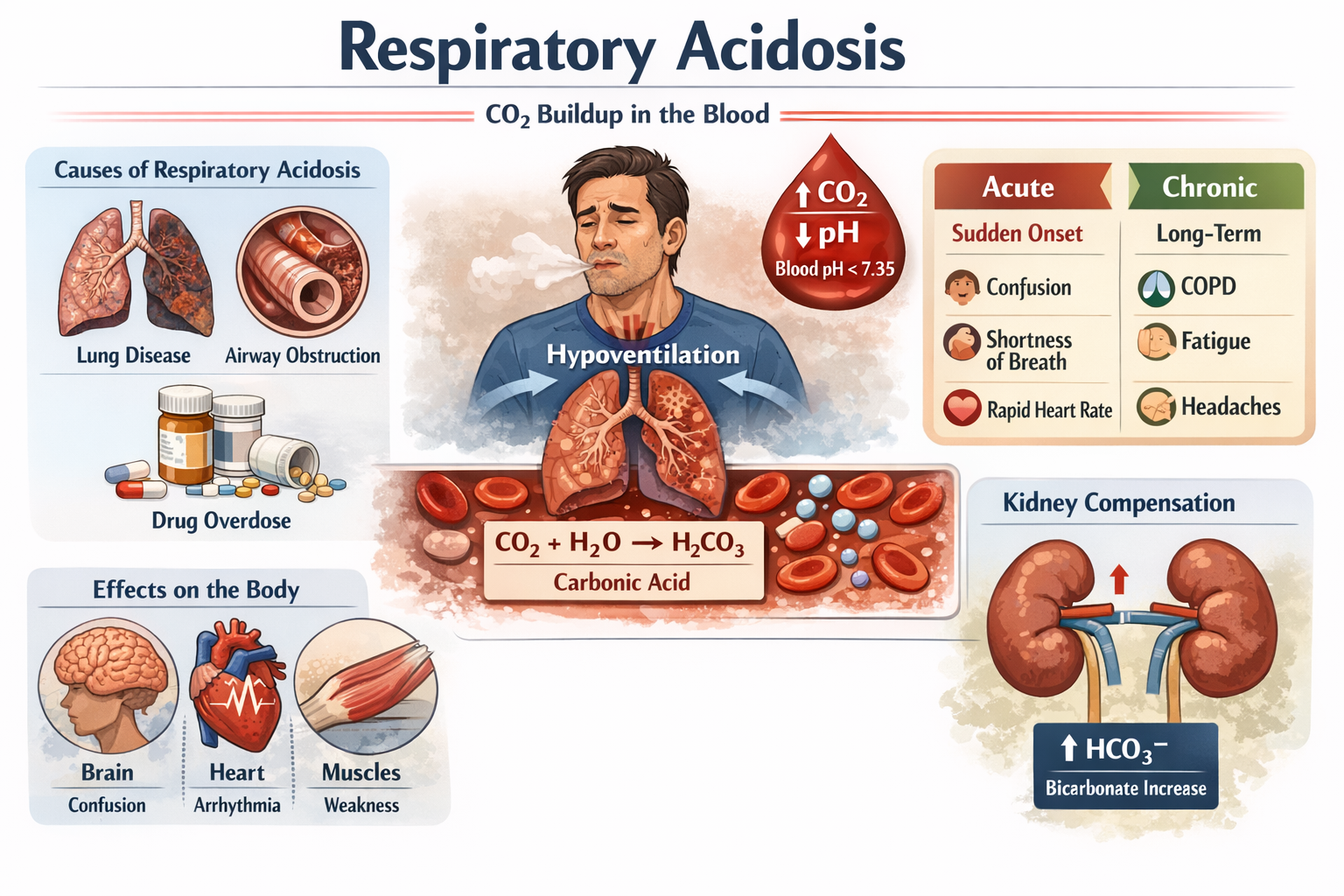
Respiratory acidosis is a medical condition that occurs when the lungs are unable to remove enough carbon dioxide (CO2) from the body, leading to an excess of CO2 in the blood. This buildup causes the blood to become more acidic than normal, lowering the blood pH below the typical range of 7.35–7.45. Essentially, the body’s delicate acid-base balance is disrupted, which can have significant effects on organ function, especially the heart and brain.
Definition of Respiratory Acidosis
In simple terms, respiratory acidosis is the result of impaired breathing, where the lungs cannot expel CO2 efficiently. Unlike metabolic acidosis, which originates from problems in the kidneys or metabolic processes, respiratory acidosis is directly linked to the respiratory system. When the lungs fail to remove CO2, the blood becomes acidic, which can affect muscle function, nerve activity, and overall body chemistry.
How Respiratory Acidosis Occurs
The primary mechanism behind respiratory acidosis is hypoventilation, or slow and ineffective breathing. Normally, breathing removes CO2, a waste product of metabolism. However, when ventilation is inadequate, CO2 accumulates in the bloodstream, forming carbonic acid, which lowers blood pH. This imbalance triggers the kidneys to compensate by increasing bicarbonate production, but this process is slower in acute cases, which is why early detection is crucial.
Acute vs Chronic Respiratory Acidosis
Respiratory acidosis can be acute or chronic, depending on how quickly it develops and how long it persists.
- Acute Respiratory Acidosis:
- Develops suddenly and is usually caused by severe lung conditions, drug overdose, or airway obstruction.
- Symptoms appear quickly, including confusion, shortness of breath, and rapid heartbeat.
- Requires immediate medical attention to prevent life-threatening complications.
- Chronic Respiratory Acidosis:
- Develops gradually over time, often due to chronic obstructive pulmonary disease (COPD), long-term asthma, or neuromuscular disorders.
- The body partially compensates by increasing bicarbonate levels in the blood, so symptoms are often milder or subtle, such as fatigue or mild headaches.
Causes of Respiratory Acidosis
Respiratory acidosis occurs when the lungs fail to remove carbon dioxide (CO2) efficiently, causing the blood to become acidic. Understanding the causes of respiratory acidosis is essential for prevention, early detection, and effective treatment. These causes can range from common respiratory conditions to less frequent underlying medical issues.
Common Causes of Respiratory Acidosis
- Chronic Obstructive Pulmonary Disease (COPD):
COPD, including emphysema and chronic bronchitis, is one of the most frequent causes of chronic respiratory acidosis. Damage to the airways and alveoli reduces the lungs’ ability to expel CO2 efficiently, gradually increasing acidity in the blood. - Severe Asthma Attacks:
During acute asthma attacks, the airways constrict, making it difficult to breathe. This hypoventilation leads to CO2 retention, causing acute respiratory acidosis if untreated. - Pneumonia:
Pneumonia causes inflammation and fluid buildup in the lungs, limiting oxygen intake and CO2 removal. This can trigger acute respiratory acidosis, especially in elderly patients or those with pre-existing lung conditions. - Pulmonary Edema:
Fluid accumulation in the lungs, often due to heart failure, reduces gas exchange efficiency. This can result in CO2 retention and subsequent respiratory acidosis. - Obstructive Sleep Apnea:
During sleep apnea episodes, breathing temporarily stops, reducing CO2 clearance. Repeated episodes can contribute to chronic respiratory acidosis over time.
Less Common Causes of Respiratory Acidosis
- Neuromuscular Disorders:
Conditions like muscular dystrophy, amyotrophic lateral sclerosis (ALS), or Guillain-Barré syndrome can weaken respiratory muscles, impairing ventilation and causing CO2 buildup. - Drug Overdose:
Overdose of sedatives, opioids, or anesthetics can slow or stop breathing, leading to acute respiratory acidosis. - Chest Wall Deformities:
Severe scoliosis or trauma to the chest wall can restrict lung expansion, reducing ventilation efficiency. - Trauma or Injury Affecting the Respiratory System:
Injuries to the spinal cord or brain can impair the nerves controlling breathing, causing CO2 retention.
Risk Factors for Respiratory Acidosis
Several factors increase the likelihood of developing respiratory acidosis:
- Smoking and Air Pollution Exposure: Damages the lungs and reduces gas exchange efficiency.
- Pre-existing Lung or Heart Disease: Conditions like COPD, asthma, and heart failure make the lungs more vulnerable.
- Advanced Age: Lung function declines naturally with age, increasing risk.
- Obesity: Can contribute to hypoventilation and sleep apnea, leading to CO2 retention.
Key Takeaway: Identifying the causes of respiratory acidosis is crucial for both prevention and treatment. While some causes are acute and potentially life-threatening, others develop slowly and may require long-term management strategies.
Symptoms of Respiratory Acidosis
Respiratory acidosis can manifest in various ways depending on whether it is acute or chronic. Recognizing the symptoms early is essential for timely intervention and preventing complications. Symptoms result primarily from the excess carbon dioxide in the blood and the resulting acid-base imbalance, which can affect the brain, heart, and muscles.
Early Warning Signs
In the initial stages, especially in chronic respiratory acidosis, symptoms may be subtle and easily overlooked:
- Shortness of Breath (Dyspnea): Difficulty in breathing, especially during physical activity.
- Fatigue and Drowsiness: General tiredness and lack of energy due to inadequate oxygen delivery to tissues.
- Headache and Confusion: Mild headaches or difficulty concentrating caused by increased CO2 levels affecting brain function.
- Restlessness or Anxiety: Feelings of unease due to the body sensing low oxygen levels.
These early warning signs are often mistaken for other respiratory or neurological conditions, which is why proper medical evaluation is important.
Severe Symptoms
In acute respiratory acidosis or advanced chronic cases, symptoms become more pronounced and potentially life-threatening:
- Rapid or Shallow Breathing: The body attempts to compensate for high CO2 levels.
- Irregular Heartbeat (Arrhythmia): Acidic blood can interfere with heart function.
- Muscle Tremors or Weakness: CO2 buildup affects nerve and muscle function.
- Confusion or Disorientation: Severe hypercapnia can impair brain function.
- Seizures or Loss of Consciousness: In extreme cases, untreated respiratory acidosis can lead to coma.
Symptoms in Chronic vs Acute Cases
| Feature | Acute Respiratory Acidosis | Chronic Respiratory Acidosis |
|---|---|---|
| Onset | Sudden | Gradual |
| Symptoms | Severe shortness of breath, confusion, arrhythmia | Mild fatigue, headaches, subtle breathlessness |
| Body Compensation | Minimal | Kidneys partially compensate by increasing bicarbonate |
| Urgency | Medical emergency | Manageable with ongoing treatment |
Key Takeaway: Symptoms of respiratory acidosis vary based on duration and severity. Early detection can prevent serious complications, while chronic cases require long-term monitoring and management.
How Respiratory Acidosis is Diagnosed
Diagnosing respiratory acidosis requires careful evaluation of symptoms, medical history, and laboratory tests. Since the condition directly affects blood pH and carbon dioxide levels, accurate diagnosis is critical for timely and effective treatment.
Blood Tests
The most important diagnostic tool for respiratory acidosis is the arterial blood gas (ABG) test. This test measures:
- pH Levels: Normal blood pH ranges from 7.35–7.45. A lower pH indicates acidosis.
- Partial Pressure of Carbon Dioxide (PaCO2): Elevated CO2 confirms hypoventilation.
- Bicarbonate (HCO3−) Levels: Helps differentiate between acute and chronic respiratory acidosis, as chronic cases often show compensatory increases in bicarbonate.
Key Insight: ABG testing provides a direct measurement of blood acidity and CO2 retention, making it the gold standard for diagnosing respiratory acidosis.
Pulmonary Function Tests
Pulmonary function tests (PFTs) assess how well the lungs are moving air and exchanging gases. These tests are particularly useful for chronic respiratory acidosis caused by conditions like COPD or neuromuscular disorders. PFTs may include:
- Spirometry: Measures airflow and lung volume.
- Lung Volume Tests: Determines how much air remains in the lungs after exhaling.
- Diffusion Capacity: Checks how efficiently oxygen moves from the lungs into the blood.
By evaluating lung efficiency, doctors can identify the underlying cause of CO2 retention.
Imaging and Other Diagnostic Tools
Imaging techniques help detect structural or infectious causes of respiratory acidosis:
- Chest X-ray: Identifies pneumonia, pulmonary edema, or lung deformities.
- CT Scan: Provides a more detailed view of lung tissue and airways.
- Electrocardiogram (ECG): May be used to check for heart complications related to acidosis.
Additional Tests: For patients suspected of having sleep apnea or neuromuscular disorders, sleep studies or nerve conduction tests may also be recommended.
Key Takeaway: Proper diagnosis of respiratory acidosis involves a combination of blood tests, pulmonary assessments, and imaging. Early detection enables effective treatment and reduces the risk of severe complications.
Complications of Respiratory Acidosis
If left untreated, respiratory acidosis can lead to serious short-term and long-term complications. The severity depends on whether the condition is acute or chronic, the underlying cause, and how quickly treatment begins. Understanding potential complications underscores the importance of early diagnosis and ongoing management.
Short-term Complications
Acute respiratory acidosis can develop rapidly and may cause immediate health risks, such as:
- Heart Rhythm Problems (Arrhythmias): Elevated CO2 levels and acidic blood can disrupt the electrical activity of the heart, potentially causing irregular heartbeat or cardiac arrest.
- Confusion or Fainting: The brain is highly sensitive to blood pH changes. Rapid CO2 buildup can impair cognitive function, leading to disorientation, dizziness, or fainting.
- Respiratory Failure: Severe hypoventilation can reduce oxygen levels drastically, potentially requiring emergency ventilation.
Short-term complications are life-threatening and require immediate medical attention.
Long-term Complications
Chronic respiratory acidosis develops slowly, and while symptoms may be subtle, prolonged CO2 retention can have lasting effects:
- Chronic Respiratory Failure: Long-term hypoventilation weakens the lungs, making it harder to breathe over time.
- Organ Dysfunction: Persistent acidity in the blood can damage organs, especially the heart and kidneys.
- Cognitive Impairment: Chronic high CO2 levels can affect memory, concentration, and overall brain function.
- Pulmonary Hypertension: High pressure in the pulmonary arteries can develop due to ongoing lung stress.
How Early Treatment Can Prevent Complications
Prompt identification and treatment of respiratory acidosis can prevent many of these complications:
- Oxygen therapy improves blood oxygen levels and supports lung function.
- Medication for underlying conditions like COPD or infections reduces CO2 retention.
- Lifestyle changes, including quitting smoking and maintaining a healthy weight, support long-term lung health.
Key Takeaway: Respiratory acidosis, if untreated, can lead to serious health consequences. Early diagnosis and proper management are critical to prevent both short-term and long-term complications.
Treatment Options for Respiratory Acidosis
Treatment for respiratory acidosis focuses on addressing the underlying cause, correcting the blood acidity, and preventing further complications. The approach depends on whether the condition is acute or chronic and the severity of symptoms.
Immediate Medical Interventions
For acute respiratory acidosis, rapid intervention is critical:
- Oxygen Therapy: Administering supplemental oxygen can help maintain proper oxygen levels in the blood. Care must be monitored carefully in patients with COPD to avoid suppressing their natural breathing drive.
- Mechanical Ventilation: In severe cases, ventilators may be used to assist or take over breathing temporarily, allowing CO2 levels to normalize quickly.
- Treating Underlying Causes: Acute infections, airway obstructions, or drug overdoses are addressed immediately to restore proper lung function.
Key Insight: Immediate interventions are crucial in preventing life-threatening complications like arrhythmias, brain dysfunction, or respiratory failure.
Medications
Certain medications help manage the conditions that cause respiratory acidosis:
- Bronchodilators: For asthma or COPD patients, inhalers or nebulizers improve airflow and reduce CO2 retention.
- Antibiotics or Antivirals: Used to treat infections such as pneumonia, which can impair lung function.
- Diuretics: For patients with pulmonary edema, these medications help remove excess fluid from the lungs.
- Reversal Agents: In cases of drug overdose, specific medications may reverse respiratory depression caused by opioids or sedatives.
Lifestyle and Home Management
For chronic respiratory acidosis, long-term lifestyle adjustments can help manage the condition:
- Quit Smoking: Smoking damages the lungs and worsens CO2 retention.
- Regular Exercise: Moderate activity strengthens respiratory muscles and improves lung efficiency.
- Pulmonary Rehabilitation: Structured programs for COPD patients improve breathing and quality of life.
- Avoiding Lung Irritants: Reducing exposure to pollutants, dust, or allergens prevents flare-ups.
Managing Chronic Respiratory Acidosis
Patients with chronic conditions may require ongoing monitoring and supportive therapies:
- Home Oxygen Therapy: Helps maintain oxygen levels and reduce CO2 retention in severe COPD cases.
- Regular Checkups: Periodic ABG tests, lung function tests, and doctor consultations help track disease progression.
- Medication Adherence: Consistently using prescribed bronchodilators or other medications prevents complications.
Key Takeaway: Treatment for respiratory acidosis is multifaceted, involving emergency interventions for acute cases, medications to treat underlying causes, and lifestyle management for chronic cases. Early and consistent treatment greatly improves patient outcomes.
Prevention of Respiratory Acidosis
Preventing respiratory acidosis focuses on maintaining healthy lung function, managing chronic conditions, and avoiding factors that impair breathing. While some causes, like genetic neuromuscular disorders, cannot be fully prevented, many cases can be avoided or minimized with proactive measures.
Healthy Lung Habits
Maintaining lung health is crucial to prevent CO2 retention and respiratory acidosis:
- Quit Smoking: Smoking damages alveoli, reduces lung efficiency, and increases the risk of chronic respiratory acidosis.
- Avoid Pollutants and Allergens: Reduce exposure to air pollution, dust, and chemical fumes that can irritate the lungs.
- Practice Proper Breathing Techniques: Techniques like diaphragmatic breathing can improve oxygen intake and carbon dioxide elimination.
Managing Chronic Conditions
Patients with pre-existing respiratory or neuromuscular disorders should take active steps to prevent respiratory acidosis:
- Proper COPD or Asthma Management: Follow prescribed medications, inhalers, and pulmonary rehabilitation plans.
- Sleep Apnea Treatment: Use CPAP or other devices as recommended to prevent CO2 buildup during sleep.
- Regular Monitoring: Keep track of lung function and oxygen levels through periodic checkups.
Regular Health Checkups
Early detection of impaired lung function or CO2 retention can prevent progression to respiratory acidosis:
- Routine Blood Tests: Periodic ABG testing for at-risk patients helps identify rising CO2 levels early.
- Pulmonary Function Tests: Assess lung efficiency regularly, especially in chronic lung disease patients.
- Vaccinations: Stay up-to-date on vaccines like influenza and pneumonia to reduce risk of infections that can trigger respiratory acidosis
What is the difference between respiratory and metabolic acidosis?
Respiratory acidosis occurs when the lungs fail to remove enough carbon dioxide, leading to increased acidity in the blood. Metabolic acidosis, on the other hand, originates from the kidneys or metabolic processes, where the body produces too much acid or loses too much bicarbonate. Both affect blood pH but have different underlying causes and treatments.
Can respiratory acidosis be cured completely?
The cure for respiratory acidosis depends on its cause:
- Acute respiratory acidosis can often be resolved completely with prompt treatment, such as oxygen therapy or addressing airway obstruction.
- Chronic respiratory acidosis caused by long-term lung disease may not be fully reversible, but symptoms can be managed effectively with medications, lifestyle changes, and ongoing monitoring.
How quickly can respiratory acidosis become life-threatening?
Acute respiratory acidosis can become life-threatening within hours if CO2 levels rise rapidly. Severe hypercapnia can lead to respiratory failure, cardiac arrhythmias, or coma, making early detection and emergency treatment critical. Chronic respiratory acidosis usually develops slowly, giving more time for management.
Are there natural ways to support lung function?
Yes, natural methods can help maintain healthy lungs and reduce the risk of respiratory acidosis:
- Regular aerobic exercise to strengthen respiratory muscles.
- Deep breathing exercises such as diaphragmatic breathing.
- Maintaining a healthy weight to reduce strain on the lungs.
- Avoiding smoking and polluted environments.
Which tests are most reliable for diagnosing respiratory acidosis?
The most reliable tests include:
- Arterial Blood Gas (ABG) Test: Directly measures blood pH, CO2, and bicarbonate levels.
- Pulmonary Function Tests (PFTs): Assess lung efficiency and airflow.
- Imaging (X-ray or CT Scan): Detects underlying lung conditions like pneumonia or pulmonary edema.
Conclusion
Respiratory acidosis is a serious condition that occurs when the lungs cannot remove enough carbon dioxide, causing the blood to become too acidic. Understanding the causes of respiratory acidosis, including chronic lung diseases like COPD, acute conditions like severe asthma attacks, and other less common factors, is essential for early detection and prevention.
The symptoms can vary from mild fatigue and headaches in chronic cases to confusion, arrhythmias, or respiratory failure in acute situations. Accurate diagnosis through blood tests, pulmonary function tests, and imaging is crucial to identify the severity and underlying cause of the condition.
Treatment strategies range from emergency interventions, such as oxygen therapy and mechanical ventilation, to long-term management through medications, lifestyle changes, and pulmonary rehabilitation. Preventive measures like quitting smoking, maintaining healthy lung habits, and regular checkups can significantly reduce the risk of developing respiratory acidosis or its complications.