Introduction
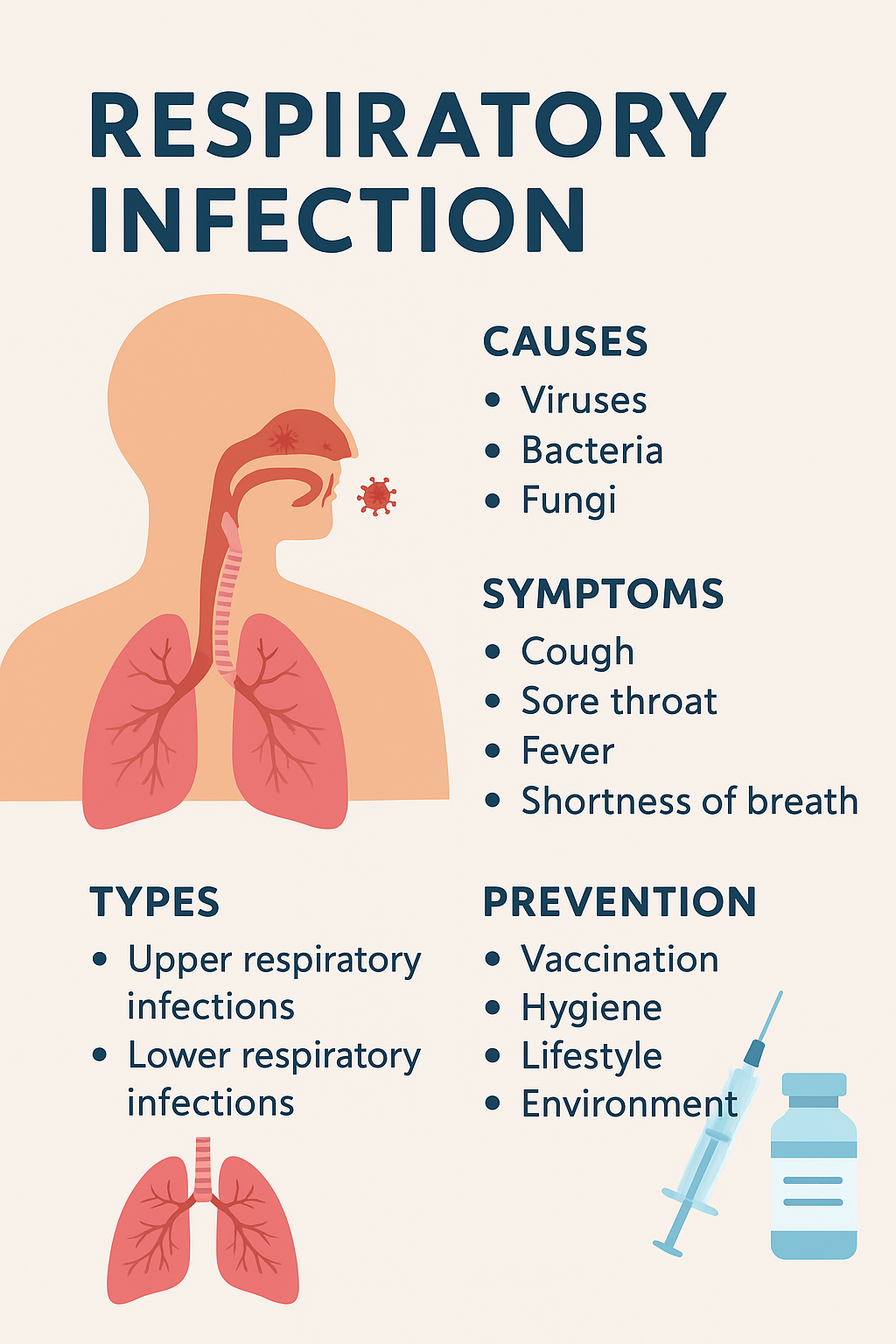
Respiratory infections are among the most common health problems worldwide, affecting millions of people each year. A respiratory infection occurs when viruses, bacteria, or other pathogens invade the respiratory tract, which includes the nose, throat, airways, and lungs. These infections can range from mild illnesses, like the common cold, to severe conditions, such as pneumonia or tuberculosis.
Understanding respiratory infections is crucial because early recognition of symptoms and proper treatment can prevent complications, especially in vulnerable groups like children, the elderly, and people with weakened immune systems. In this article, we will cover everything you need to know about respiratory infections—including causes, symptoms, types, treatments, prevention strategies, and frequently asked questions. By the end, you’ll have a clear understanding of how to protect yourself and manage these infections effectively.
What is a Respiratory Infection?
A respiratory infection is an illness that affects any part of the respiratory system, including the nose, throat, airways, and lungs. These infections occur when harmful microorganisms, such as viruses, bacteria, or fungi, enter the respiratory tract and cause inflammation. Respiratory infections are extremely common and can affect people of all ages, although certain groups—like infants, older adults, and individuals with weakened immune systems—are more susceptible to severe forms.
Upper vs. Lower Respiratory Infections
Respiratory infections are generally classified into upper and lower respiratory infections based on the part of the respiratory system they affect:
- Upper Respiratory Infections (URIs): These infections affect the nose, sinuses, and throat. Common URIs include:
- Common cold – caused by viruses like rhinovirus
- Sinusitis – infection of the sinuses
- Pharyngitis and laryngitis – inflammation of the throat and voice box
- Lower Respiratory Infections (LRIs): These infections affect the airways and lungs and are generally more serious. Examples include:
- Bronchitis – inflammation of the bronchial tubes
- Pneumonia – infection of the lungs that can be viral, bacterial, or fungal
- Tuberculosis (TB) – a chronic bacterial lung infection
Common Types of Respiratory Infections
Respiratory infections can be caused by different types of pathogens:
- Viral respiratory infections: Influenza, COVID-19, RSV, and common cold viruses
- Bacterial respiratory infections: Streptococcus pneumoniae, Haemophilus influenzae, and Mycoplasma pneumoniae
- Fungal infections: Rare but can affect immunocompromised individuals
Understanding the type of infection is critical because it determines the treatment plan. For example, antibiotics are effective only for bacterial infections, not viral ones.
Why Respiratory Infections Matter
While many respiratory infections are mild and self-limiting, they can lead to serious complications if not properly managed. Severe respiratory infections can cause difficulty breathing, organ damage, or even death in high-risk individuals. Early recognition of symptoms, proper hygiene, vaccination, and timely medical care are essential in reducing the impact of these infections.
Causes of Respiratory Infections
Respiratory infections can arise from various causes, primarily viruses, bacteria, fungi, and environmental factors. Understanding the root cause helps in prevention, early diagnosis, and effective treatment.
Viral Causes of Respiratory Infections
Viruses are the most common cause of respiratory infections, responsible for illnesses ranging from the common cold to severe pneumonia. Common viral pathogens include:
- Influenza virus – Causes seasonal flu with fever, body aches, cough, and fatigue. Influenza can lead to complications like pneumonia, especially in children and older adults.
- Coronavirus (including COVID-19) – Can infect both upper and lower respiratory tracts, causing symptoms like fever, cough, and shortness of breath. Severe cases may require hospitalization.
- Respiratory syncytial virus (RSV) – Often affects infants and young children, causing bronchiolitis and pneumonia.
- Rhinovirus and adenovirus – Major causes of the common cold, typically mild but highly contagious.
Bacterial Causes of Respiratory Infections
Bacterial infections can be more severe than viral ones and often require antibiotics for treatment. Common bacterial causes include:
- Streptococcus pneumoniae – Can cause pneumonia, sinus infections, and ear infections.
- Haemophilus influenzae – Often linked to bronchitis and pneumonia, particularly in people with weakened immune systems.
- Mycoplasma pneumoniae – Causes “walking pneumonia,” a milder but persistent form of lung infection.
Fungal and Other Causes
Although less common, fungi can also cause respiratory infections, especially in individuals with compromised immune systems. Examples include:
- Aspergillus species – Can lead to lung infections in immunocompromised patients
- Histoplasma capsulatum – Causes histoplasmosis, often associated with exposure to bird or bat droppings
Environmental and Lifestyle Risk Factors
Several non-infectious factors can increase susceptibility to respiratory infections:
- Smoking and exposure to secondhand smoke – Damages airways and weakens immune defense
- Air pollution – Particulate matter irritates the lungs, making infections more likely
- Weakened immune system – Due to chronic diseases, stress, or certain medications
- Close contact with infected individuals – Crowded places, schools, or healthcare settings
Symptoms of Respiratory Infections
Recognizing the symptoms of a respiratory infection early is essential for effective treatment and preventing complications. Symptoms can vary depending on whether the infection affects the upper or lower respiratory tract, and whether it is viral, bacterial, or fungal.
Common Symptoms of Respiratory Infections
Most respiratory infections start with mild, easily noticeable symptoms, such as:
- Cough – Can be dry or produce mucus, depending on the type of infection
- Sore throat – Often accompanies viral infections like the common cold or pharyngitis
- Runny or congested nose – Typical in upper respiratory infections
- Fever and chills – Usually mild in viral infections, but can be higher in bacterial infections
- Fatigue and body aches – Common during viral illnesses like influenza
Other general symptoms may include headache, mild shortness of breath, and watery eyes. These early signs often resolve within a few days with rest and home care for mild infections.
Severe Symptoms Requiring Medical Attention
In some cases, respiratory infections can escalate and become life-threatening. Seek immediate medical care if you notice:
- Shortness of breath or difficulty breathing – May indicate pneumonia or severe bronchitis
- Chest pain or pressure – Can signal a serious lower respiratory infection
- Persistent high fever – Especially if lasting more than 3 days
- Confusion, dizziness, or extreme fatigue – Particularly in elderly patients or infants
- Bluish lips or face – A sign of oxygen deprivation
Severe infections can develop rapidly, especially in high-risk populations like children, older adults, and immunocompromised individuals. Early medical intervention can significantly reduce complications.
Symptoms by Infection Type
| Infection Type | Typical Symptoms | Severity Level |
|---|---|---|
| Common Cold (Viral URI) | Runny nose, sneezing, mild cough | Mild |
| Influenza (Viral LRI) | High fever, body aches, cough, fatigue | Moderate to Severe |
| Pneumonia (Bacterial or Viral LRI) | Chest pain, persistent cough, high fever, shortness of breath | Severe |
| Tuberculosis (Bacterial LRI) | Persistent cough, night sweats, weight loss, fatigue | Severe, chronic |
Types of Respiratory Infections
Respiratory infections are broadly classified into upper respiratory infections (URIs) and lower respiratory infections (LRIs). Understanding the differences between these types helps in diagnosis, treatment, and prevention.
Upper Respiratory Infections (URIs)
Upper respiratory infections affect the nose, sinuses, throat, and larynx. They are generally mild and resolve within a week or two but can still cause discomfort and affect daily activities. Common URIs include:
- Common Cold – Caused by viruses like rhinovirus and adenovirus; symptoms include runny nose, sneezing, and mild fever.
- Sinusitis – Infection of the sinuses leading to congestion, facial pain, and headache.
- Pharyngitis – Inflammation of the throat, often accompanied by sore throat and difficulty swallowing.
- Laryngitis – Affects the voice box, causing hoarseness and voice loss.
Key Points About URIs:
- Usually viral in nature
- Mild and self-limiting
- Can be prevented with good hygiene and vaccination (for influenza)
Lower Respiratory Infections (LRIs)
Lower respiratory infections affect the airways and lungs and are often more serious than URIs. LRIs can lead to hospitalization, especially in vulnerable populations. Common LRIs include:
- Bronchitis – Inflammation of the bronchial tubes, causing persistent cough, mucus production, and sometimes mild fever.
- Pneumonia – Infection of the lungs that can be viral, bacterial, or fungal; symptoms include chest pain, high fever, and severe shortness of breath.
- Tuberculosis (TB) – Chronic bacterial infection causing persistent cough, night sweats, weight loss, and fatigue; requires long-term antibiotic treatment.
Key Points About LRIs:
- Can be bacterial, viral, or fungal
- Often require medical treatment
- Can cause severe complications if untreated
Other Specific Respiratory Infections
- RSV (Respiratory Syncytial Virus): Common in infants and young children, causing bronchiolitis and pneumonia.
- Influenza (Flu): Seasonal viral infection affecting both upper and lower respiratory tracts.
- COVID-19: Can range from mild cold-like symptoms to severe pneumonia and respiratory failure.
Diagnosis of Respiratory Infections
Proper diagnosis of respiratory infections is essential to determine the cause—whether viral, bacterial, or fungal—and to provide the correct treatment. Doctors use a combination of physical examination, patient history, laboratory tests, and imaging to make an accurate diagnosis.
Physical Examination and Patient History
- Doctors first assess symptoms such as cough, fever, shortness of breath, and chest pain.
- They check for signs of respiratory distress, like rapid breathing or wheezing.
- Medical history helps identify risk factors such as chronic illnesses, smoking, immunodeficiency, or recent exposure to infected individuals.
Laboratory Tests
- Blood Tests: Can indicate infection and inflammation by measuring white blood cell count.
- Throat or Nasal Swabs: Identify specific viruses or bacteria causing the infection.
- Sputum Tests: Examining mucus coughed up from the lungs helps detect bacterial or fungal pathogens.
Imaging Tests
- Chest X-ray: Used to detect pneumonia, lung inflammation, or fluid accumulation.
- CT Scan: Provides a detailed view of the lungs and is used for complex or severe infections.
Differentiating Viral and Bacterial Infections
- Viral infections often present with milder symptoms, such as low-grade fever and fatigue, and usually improve on their own.
- Bacterial infections are more likely to cause high fever, severe cough, and prolonged illness, and often require antibiotics.
- Sometimes, doctors may use rapid antigen tests or PCR tests to identify the specific pathogen.
Other Diagnostic Considerations
- Underlying Conditions: Patients with asthma, COPD, or weakened immunity may require additional tests.
- Severity Assessment: Determines whether outpatient treatment is sufficient or hospitalization is necessary.
Treatment Options for Respiratory Infections
Treating a respiratory infection depends on its cause, severity, and the patient’s overall health. Mild infections often resolve with home care, while severe bacterial or viral infections may require medical intervention.
Home Remedies and Self-Care
For mild respiratory infections, self-care measures can significantly reduce symptoms and speed recovery:
- Rest and hydration: Adequate sleep and drinking plenty of fluids help the immune system fight infections.
- Warm fluids and steam inhalation: Tea, soups, and steam from a hot shower or humidifier can soothe the throat and clear nasal congestion.
- Over-the-counter medications: Pain relievers, fever reducers, and decongestants can ease discomfort.
- Saltwater gargle: Helps relieve sore throat and reduce inflammation.
These measures are particularly effective for viral upper respiratory infections, like the common cold.
Medical Treatment
When infections are more severe or bacterial in origin, medical treatments are necessary:
- Antibiotics: Prescribed only for bacterial infections such as bacterial pneumonia, strep throat, or TB. Overuse can lead to antibiotic resistance.
- Antiviral medications: Certain viral infections, such as influenza or severe COVID-19 cases, may require antiviral drugs.
- Hospitalization: Severe lower respiratory infections, like pneumonia or complications from influenza, may require oxygen therapy, IV fluids, or intensive care.
Managing Complications
Some respiratory infections can lead to complications if untreated:
- Pneumonia: Can develop from both viral and bacterial infections, leading to lung inflammation and difficulty breathing.
- Asthma or COPD flare-ups: Respiratory infections often exacerbate chronic lung conditions.
- Sepsis: Rare but serious bacterial infections can spread into the bloodstream.
Monitoring and Follow-Up:
- Patients recovering from severe respiratory infections should have follow-up appointments to ensure lungs are healing properly.
- Vaccinations and preventive measures are recommended to reduce the risk of future infections.
Prevention of Respiratory Infections
Preventing respiratory infections is often easier than treating them, and it involves a combination of vaccination, hygiene practices, and healthy lifestyle habits. Implementing these measures reduces the risk of infection and helps protect vulnerable populations.
Vaccinations
Vaccines play a critical role in preventing serious respiratory infections:
- Influenza vaccine: Recommended annually to protect against seasonal flu strains.
- COVID-19 vaccine: Reduces the risk of severe respiratory illness caused by coronavirus.
- Pneumococcal vaccine: Protects against pneumonia caused by Streptococcus pneumoniae, especially for older adults and high-risk individuals.
- Other vaccines: TB vaccination (BCG) in certain countries and RSV vaccines for infants in development.
Good Hygiene Practices
Simple hygiene measures significantly lower the risk of spreading infections:
- Regular handwashing with soap and water
- Using hand sanitizers when soap isn’t available
- Covering mouth and nose when coughing or sneezing
- Avoiding close contact with sick individuals
Healthy Lifestyle and Immune Support
A strong immune system helps the body fight infections:
- Balanced diet: Rich in vitamins C, D, and zinc
- Regular exercise: Enhances immune response
- Adequate sleep: Rest supports recovery and immune function
- Avoiding smoking and pollutants: Reduces airway irritation and vulnerability
Common Myths and Misconceptions About Respiratory Infections
Respiratory infections are surrounded by several myths and misconceptions that can lead to improper treatment or preventable spread. Understanding the facts helps in managing and preventing infections effectively.
Myth 1: Antibiotics Cure All Respiratory Infections
- Fact: Antibiotics are effective only against bacterial infections.
- Viral infections, like the common cold, influenza, or most cases of bronchitis, cannot be treated with antibiotics. Using antibiotics unnecessarily can lead to antibiotic resistance.
Myth 2: Cold Weather Causes Respiratory Infections
- Fact: Cold weather itself does not directly cause infections.
- Respiratory infections are caused by viruses or bacteria. However, cold weather can weaken the immune system and encourage people to stay indoors, increasing exposure to infected individuals.
Myth 3: All Coughs Indicate a Serious Infection
- Fact: Most coughs are due to mild viral infections or irritants.
- Persistent or severe coughs, especially with fever or shortness of breath, may indicate a serious lower respiratory infection and require medical attention.
Myth 4: You Can Only Get Respiratory Infections Once Per Season
- Fact: There are many strains of viruses and bacteria, so it’s possible to catch multiple infections in a season.
- Vaccinations and hygiene practices reduce risk but do not guarantee complete immunity.
Myth 5: Over-the-Counter Medications Can Cure Infections
- Fact: OTC medications help relieve symptoms but do not cure the infection.
- They are useful for comfort but should be combined with rest, hydration, and medical treatment if necessary.
When to See a Doctor
While many respiratory infections are mild and resolve on their own, it is important to recognize when professional medical care is necessary. Early medical intervention can prevent complications and, in some cases, be life-saving.
Warning Signs of Severe Infection
Seek medical attention if you experience any of the following:
- Shortness of breath or difficulty breathing – May indicate pneumonia or another severe lower respiratory infection.
- Persistent high fever – Especially if it lasts more than 3 days or is above 102°F (39°C).
- Chest pain or pressure – Could signal a serious lung infection.
- Confusion or extreme fatigue – Particularly concerning in elderly patients or infants.
- Bluish lips or face – A sign of oxygen deprivation and a medical emergency.
High-Risk Groups Who Should Be Extra Cautious
Certain individuals are more likely to develop complications from respiratory infections:
- Infants and young children – Their immune systems are still developing.
- Elderly adults – Age-related immune decline increases risk.
- Immunocompromised individuals – Including people with HIV, cancer, or those taking immunosuppressive drugs.
- People with chronic lung conditions – Such as asthma or COPD.
Tips for Seeking Care
- Do not ignore symptoms: Even mild symptoms can worsen in high-risk populations.
- Follow medical advice: Take prescribed medications fully and attend follow-up appointments.
- Monitor at home: Track fever, breathing difficulties, and oxygen levels if recommended by a healthcare provider.
Prevention and Protection Against Respiratory Infections
Preventing respiratory infections is often easier than treating them, and simple daily habits can significantly reduce the risk of catching or spreading illnesses. While no measure is 100% foolproof, combining multiple strategies offers the best protection.
1. Vaccinations
Vaccines remain one of the most effective ways to prevent serious respiratory infections:
- Influenza vaccine – Recommended annually for everyone over 6 months of age.
- COVID-19 vaccine – Helps reduce severity and risk of hospitalization.
- Pneumococcal vaccines – Particularly important for infants, older adults, and those with chronic conditions.
- Whooping cough (Tdap) booster – Protects against pertussis, which can be severe in infants and the elderly.
2. Good Hygiene Practices
Maintaining hygiene is crucial to preventing respiratory infections:
- Frequent handwashing with soap and water for at least 20 seconds.
- Use of hand sanitizer containing at least 60% alcohol when soap is unavailable.
- Avoid touching your face, particularly the eyes, nose, and mouth.
- Covering coughs and sneezes with a tissue or elbow to prevent droplet spread.
3. Environmental Measures
Your surroundings can influence infection risk:
- Regularly disinfect high-touch surfaces such as doorknobs, phones, and keyboards.
- Ensure proper ventilation in homes and workplaces. Open windows when possible to allow fresh air circulation.
- Maintain clean air filters in air conditioners and heaters.
4. Healthy Lifestyle Choices
A strong immune system is your first line of defense:
- Balanced diet rich in fruits, vegetables, lean proteins, and whole grains.
- Regular exercise to boost immune function.
- Adequate sleep, aiming for 7–9 hours per night for adults.
- Stress management, as chronic stress can weaken immunity.
5. Avoiding High-Risk Situations
Certain environments increase the chance of respiratory infections:
- Crowded or poorly ventilated spaces during peak respiratory illness seasons.
- Close contact with sick individuals—if unavoidable, consider masks and frequent hand hygiene.
- Smoking and secondhand smoke exposure, which can impair lung defenses.
By combining vaccination, hygiene, environmental precautions, and lifestyle strategies, individuals can substantially reduce their risk of respiratory infections and protect vulnerable populations around them.
Home Care and Symptom Management
For mild respiratory infections, most people can recover at home with proper care and monitoring. While rest and hydration are key, managing symptoms effectively can reduce discomfort and prevent complications.
1. Rest and Activity Management
- Prioritize rest: Allow your body to focus on fighting the infection.
- Gradually resume activities: Avoid strenuous exercise until fully recovered.
- Listen to your body: Fatigue is a sign to slow down and conserve energy.
2. Hydration and Nutrition
- Drink plenty of fluids: Water, herbal teas, and broths help thin mucus and prevent dehydration.
- Eat nutrient-rich meals: Foods high in vitamins C, D, and zinc support immune function.
- Small, frequent meals: If appetite is low, smaller meals ensure energy intake without overwhelming the digestive system.
3. Symptom Relief Measures
- Fever and pain management: Use over-the-counter medications like acetaminophen or ibuprofen as directed.
- Cough relief: Honey (for adults and children over 1 year) or warm fluids can soothe the throat. Avoid suppressing productive coughs that help clear mucus.
- Nasal congestion: Saline sprays, steam inhalation, or humidifiers can ease breathing.
4. Monitoring Symptoms at Home
- Track fever and duration: Persistent high fever may indicate complications.
- Observe breathing patterns: Wheezing, shortness of breath, or rapid breathing require immediate medical attention.
- Oxygen levels (if advised): Pulse oximeters can help high-risk individuals monitor oxygen saturation.
5. When to Seek Escalated Care
Even with home management, certain symptoms necessitate medical evaluation:
- Fever lasting more than 3 days or exceeding 102°F (39°C).
- Difficulty breathing, chest pain, or wheezing.
- Confusion, severe fatigue, or bluish lips and face.
- Symptoms worsening instead of improving after 5–7 days.
6. Avoiding Spread to Others
- Stay home: Minimize contact with others while contagious.
- Practice respiratory etiquette: Cover coughs and sneezes and dispose of tissues properly.
- Disinfect shared surfaces: Reduce the risk of transmitting germs to household members.
Proper home care, combined with vigilance for warning signs, allows most respiratory infections to resolve safely without hospitalization. However, maintaining awareness of potential complications is critical, especially for high-risk groups.