Home Health Care: The Complete Guide for Patients and Families
What is Home Health Care?
Home health care refers to a range of medical and supportive services provided in the comfort of a patient’s home. Unlike care received in hospitals or assisted living facilities, home health care allows individuals to maintain independence while receiving professional medical attention and daily support. This type of care is tailored to meet the unique needs of each patient, often involving a combination of skilled nursing, therapy, and personal care services.
The main purpose of home health care is to support recovery, manage chronic illnesses, and enhance quality of life without requiring patients to leave their homes. This approach is particularly beneficial for seniors, individuals recovering from surgery or illness, and people with long-term health conditions who may find frequent hospital visits challenging or stressful.
Differences Between Home Health Care, Hospice Care, and Assisted Living
- Home Health Care: Focuses on medical and supportive services for patients who need care while living at home. Services may be short-term (after surgery) or long-term (chronic illness management).
- Hospice Care: Specialized care for patients with terminal illnesses, focusing on comfort and quality of life rather than curative treatments. Hospice can also be provided at home.
- Assisted Living: Residential facilities where individuals live full-time with access to personal care services and limited medical supervision. Assisted living is less individualized than home health care and may not meet complex medical needs.
Key Benefits of Home Health Care
- Comfort of Home: Patients receive care in a familiar environment, which can reduce stress and promote healing.
- Personalized Care Plans: Home health care providers develop individualized care plans based on patient needs and medical conditions.
- Reduced Risk of Infection: By avoiding hospital stays, patients are less exposed to infections such as MRSA or other healthcare-associated infections.
- Family Involvement: Family members can participate in care planning and daily support, which strengthens emotional support networks.
- Cost-Effectiveness: Home health care is often more affordable than long-term hospital or facility-based care, especially for ongoing or rehabilitation needs.
Fact: According to the National Association for Home Care & Hospice (NAHC), approximately 12 million patients in the U.S. receive home health care services each year, highlighting the growing demand for in-home medical support.
Types of Home Health Care Services
Home health care services encompass a broad range of medical and non-medical support, designed to meet the unique needs of patients in their own homes. Understanding these services helps families choose the right care and ensures patients receive the proper support for recovery, chronic illness management, or daily living assistance.
1. Skilled Nursing Care at Home
Skilled nursing is one of the most common home health care services. Registered nurses (RNs) or licensed practical nurses (LPNs) provide medical care that typically includes:
- Administering medications, injections, or IV therapy
- Monitoring vital signs and overall health conditions
- Wound care and management of surgical incisions
- Education for patients and families about managing illnesses at home
Case Study: A patient recovering from hip replacement surgery received skilled nursing care at home, including daily wound checks and physical therapy coordination. This resulted in faster recovery and reduced hospital readmission compared to patients who stayed in a rehabilitation facility.
2. Physical, Occupational, and Speech Therapy
Therapy services in home health care are essential for patients recovering from injuries, surgeries, or strokes.
- Physical Therapy (PT): Improves mobility, strength, balance, and reduces the risk of falls.
- Occupational Therapy (OT): Helps patients perform daily activities like dressing, bathing, and cooking independently.
- Speech Therapy: Supports patients with communication, swallowing, or cognitive issues caused by conditions such as stroke or neurological disorders.
Fact: According to the Centers for Medicare & Medicaid Services (CMS), patients who receive home therapy services show 20-30% faster functional improvement compared to traditional outpatient therapy.
3. Personal Care Assistance
Personal care services focus on daily living needs, allowing patients to remain at home safely and comfortably. Common tasks include:
- Bathing, grooming, and dressing
- Meal preparation and feeding assistance
- Mobility support and safe transfers
- Light housekeeping and laundry
These services are often provided by home health aides (HHAs), who work under supervision of nurses to ensure both safety and comfort.
4. Medication Management and Monitoring
Proper medication management is crucial for patients with chronic illnesses or complex treatment plans. Home health care providers assist with:
- Organizing medications in pillboxes or medication dispensers
- Administering medications on schedule
- Monitoring side effects or interactions
- Educating patients and families on adherence and proper usage
5. Chronic Disease Management
For patients with conditions like diabetes, heart disease, COPD, or kidney failure, home health care plays a vital role in ongoing management. Services include:
- Regular monitoring of vital signs and blood sugar levels
- Coordinating care with physicians and specialists
- Lifestyle coaching, including diet, exercise, and symptom management
- Early detection of complications to prevent hospitalizations
Table: Common Chronic Conditions and Home Health Care Interventions
| Condition | Home Health Care Services Provided | Benefits |
|---|---|---|
| Diabetes | Blood sugar monitoring, medication management, diet guidance | Reduced complications, better blood sugar control |
| Heart Disease | Vital sign monitoring, medication management, education on symptoms | Reduced hospital readmissions, improved heart health |
| Stroke | Physical, occupational, speech therapy, mobility support | Faster recovery, improved independence |
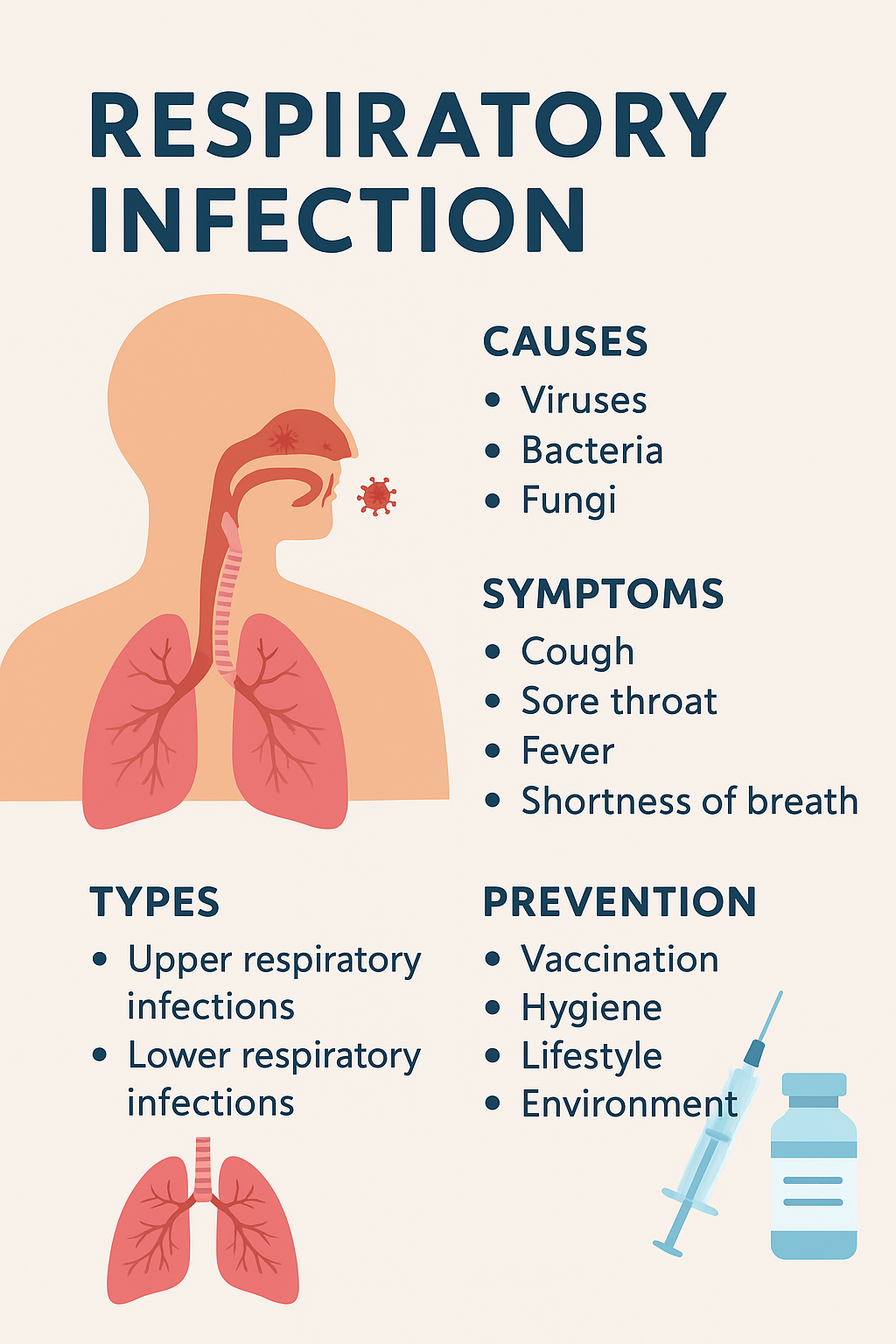
| COPD / Respiratory | Oxygen therapy supervision, medication adherence, respiratory exercises | Improved breathing, reduced exacerbations |
Home health care offers a comprehensive approach, combining medical, therapeutic, and daily living support to ensure patients remain safe, independent, and comfortable. Each service is tailored to the patient’s specific needs, creating a personalized care plan that promotes faster recovery and better long-term health outcomes.
Who Can Benefit from Home Health Care
Home health care is designed to support a wide range of patients, from seniors needing daily assistance to individuals recovering from surgery. By providing professional care at home, patients can maintain independence while receiving the medical attention and daily support they require. Understanding who benefits most from home health care helps families make informed decisions about the type and level of care needed.
1. Seniors and Elderly Patients
Older adults often face mobility challenges, chronic conditions, or cognitive decline, making home health care an ideal option. Seniors can benefit from:
- Daily health monitoring and medication management
- Assistance with personal care like bathing, dressing, and grooming
- Physical and occupational therapy to maintain mobility and prevent falls
- Companionship, reducing feelings of loneliness or isolation
Fact: According to the CDC, nearly 1 in 4 adults aged 65+ report difficulties with daily living activities, making home health care essential for maintaining quality of life.
2. People Recovering from Surgery or Illness
Patients discharged from hospitals after surgeries or acute illnesses often require continued medical supervision to ensure full recovery. Home health care helps by:
- Providing wound care, IV therapy, or pain management
- Monitoring vital signs to detect early complications
- Coordinating with doctors for follow-up care
- Assisting with mobility and daily activities to prevent hospital readmission
Example: A patient recovering from cardiac surgery received skilled nursing visits and physical therapy at home. The personalized care plan reduced the patient’s risk of complications and allowed a faster return to normal activities.
3. Individuals with Chronic Conditions
Patients with long-term conditions such as diabetes, heart disease, COPD, or kidney disease require ongoing monitoring and management. Home health care can:
- Track vital signs and symptoms regularly
- Ensure proper medication administration
- Offer lifestyle guidance on diet, exercise, and symptom management
- Provide early intervention if complications arise
Fact: Studies show that patients with chronic illnesses receiving home health care have 30% fewer hospital readmissions compared to those without in-home support.
4. Patients with Disabilities or Mobility Challenges
Individuals with physical disabilities, neurological conditions, or limited mobility often struggle with routine activities. Home health care provides:
- Assistance with personal care and mobility
- Adaptive therapies to improve function and independence
- Support for daily living activities like cooking, bathing, or transportation
Quote: According to the National Association for Home Care & Hospice, “Home health care empowers patients with disabilities to live safely at home while receiving the medical support they need.”
By catering to seniors, post-surgical patients, chronic disease sufferers, and individuals with disabilities, home health care ensures that each patient receives personalized, effective, and safe care in the comfort of their own home.
How Home Health Care Works
Home health care operates through a structured process that ensures each patient receives personalized care tailored to their medical and daily living needs. From the initial assessment to ongoing monitoring, home health care focuses on safety, recovery, and independence. Understanding the process helps families feel confident in choosing the right services.
1. Initial Assessment by a Registered Nurse
The first step in home health care is a comprehensive assessment, usually conducted by a registered nurse (RN). This evaluation determines the patient’s medical condition, daily living needs, and the type of care required. Key aspects include:
- Reviewing medical history and current medications
- Assessing mobility, strength, and cognitive function
- Evaluating home safety and accessibility
- Identifying the patient’s personal goals and preferences
Fact: A thorough initial assessment ensures that care plans are individualized, which improves outcomes and reduces hospital readmissions.
2. Developing a Personalized Care Plan
Based on the assessment, the home health care team creates a customized care plan. This plan outlines:
- Frequency and type of visits (nursing, therapy, or aide support)
- Specific medical interventions or therapies needed
- Goals for recovery, rehabilitation, or chronic disease management
- Emergency protocols and contact information
Example: For a patient recovering from hip replacement, the care plan may include daily nursing visits for wound care, physical therapy three times a week, and home safety modifications.
3. Scheduling Visits and Ongoing Monitoring
Home health care services are scheduled according to the patient’s needs, whether daily, several times a week, or monthly. During visits, caregivers and nurses:
- Perform medical assessments and administer treatments
- Update progress notes and report changes to the physician
- Adjust care plans as needed to improve outcomes
Fact: Continuous monitoring helps detect complications early, which is particularly important for patients with chronic illnesses or post-surgical recovery.
4. Coordination with Doctors and Family Members
A key feature of home health care is the collaborative approach. Care teams work closely with:
- Primary care physicians and specialists to ensure treatments are aligned with medical directives
- Family members to involve them in caregiving decisions and updates
- Pharmacists and therapists to manage medications and rehabilitation plans
This collaboration ensures seamless care, reduces hospital readmissions, and provides families peace of mind.
Home Health Care Team Members
A successful home health care program relies on a coordinated team of professionals, each contributing specialized skills to ensure patients receive comprehensive, high-quality care. Understanding the roles of each team member helps families know who to contact for specific needs and what to expect from the care process.
1. Registered Nurses (RNs)
Registered nurses are the backbone of home health care, providing skilled medical services, monitoring health conditions, and coordinating overall care. Their responsibilities include:
- Administering medications, injections, or IV therapies
- Monitoring vital signs and patient progress
- Managing chronic illnesses and wound care
- Educating patients and families on health management
Fact: Studies show that regular RN visits in home health care reduce hospital readmission rates by up to 25%, particularly for patients with chronic conditions.
2. Licensed Practical Nurses (LPNs) / Licensed Vocational Nurses (LVNs)
LPNs/LVNs work under the supervision of RNs, providing essential support for patients who need ongoing monitoring or assistance with medical tasks. Common duties include:
- Checking vital signs and documenting observations
- Administering medications and basic wound care
- Assisting patients with mobility or daily health routines
3. Home Health Aides (HHAs)
Home health aides focus primarily on personal care and assistance with daily living activities. They help patients maintain independence while ensuring safety at home. Responsibilities include:
- Bathing, grooming, and dressing assistance
- Meal preparation and feeding support
- Light housekeeping and laundry
- Mobility assistance and companionship
Example: An elderly patient with limited mobility may receive HHA support three times a day for personal care and mobility, while the RN visits twice a week for medical monitoring.
4. Physical, Occupational, and Speech Therapists
Therapists provide specialized rehabilitation services that improve patient function and independence:
- Physical Therapists (PTs): Help restore mobility, strength, and balance.
- Occupational Therapists (OTs): Assist with daily living activities like cooking, dressing, and home adaptations.
- Speech Therapists: Address communication, swallowing, and cognitive challenges.
Fact: Home therapy services contribute to faster recovery and higher functional independence compared to outpatient therapy, especially for post-surgical or stroke patients.
5. Social Workers and Care Coordinators
Social workers and care coordinators help patients and families navigate the healthcare system and access additional support:
- Connecting patients with community resources and support programs
- Counseling patients and families on emotional and mental health
- Coordinating between doctors, therapists, and caregivers for seamless care
Key Takeaway: A comprehensive home health care team combines medical, therapeutic, and personal care expertise to create a holistic support system for patients. Each member plays a critical role in ensuring safety, recovery, and independence in the home setting.
Benefits of Home Health Care
Home health care offers a wide range of benefits that go beyond basic medical care. By receiving professional support at home, patients and families experience improvements in health outcomes, emotional well-being, and overall quality of life.
1. Comfort and Familiarity of Home
One of the primary advantages of home health care is that patients can receive treatment in a familiar environment, surrounded by their own belongings and loved ones. This comfort:
- Reduces stress and anxiety often associated with hospital stays
- Promotes faster healing and recovery
- Helps maintain normal daily routines
Fact: Research indicates that patients recovering at home often experience lower stress levels and better mental well-being compared to those in institutional settings.
2. Personalized One-on-One Attention
Unlike hospitals where staff must divide attention among many patients, home health care provides individualized care plans tailored to each patient’s needs. Benefits include:
- Customized therapies and medical treatments
- Close monitoring for early detection of complications
- Ability to adjust care plans quickly based on patient progress
Example: A post-surgery patient may receive daily nursing visits, personalized physical therapy exercises, and medication management at home, ensuring faster recovery and fewer readmissions.
3. Faster Recovery and Rehabilitation
Studies show that patients recovering from surgery, stroke, or illness at home often regain mobility and independence faster than those in traditional care settings. Factors contributing to this include:
- One-on-one therapy sessions
- A comfortable, distraction-free environment
- Frequent monitoring and early intervention for complications
4. Cost-Effectiveness
Home health care is generally more affordable than long-term hospital or facility-based care, especially for ongoing medical support or chronic disease management. Costs are reduced by:
- Avoiding extended hospital stays
- Limiting emergency visits and readmissions
- Tailoring care to only the services needed
5. Reduced Risk of Infection
Hospitals and care facilities carry a higher risk of healthcare-associated infections. Home health care:
- Minimizes exposure to infectious diseases
- Reduces risk of hospital-acquired infections like MRSA or C. difficile
- Supports safer recovery, particularly for immunocompromised patients
6. Emotional and Psychological Benefits
Home health care also addresses mental and emotional well-being, which is often overlooked in medical treatment:
- Preserves independence and dignity for patients
- Reduces feelings of isolation or loneliness
- Provides family members with support and education to participate in care
Quote: According to the National Association for Home Care & Hospice, “Patients receiving care at home
How to Choose the Right Home Health Care Agency
Choosing the right home health care agency is one of the most important decisions families can make. The quality of care directly impacts recovery, safety, and overall well-being. Here’s a comprehensive guide to selecting the best provider for your needs.
1. Check Licensing and Certification
The first step is to ensure the agency is properly licensed and certified. Key points include:
- Verify state licensure and compliance with local regulations
- Look for accreditation from organizations like The Joint Commission or Community Health Accreditation Partner (CHAP)
- Certified agencies are held to higher standards of quality and safety, ensuring reliable care
2. Research Reputation and Reviews
A reputable agency will have positive feedback from patients, families, and healthcare professionals. Steps to evaluate reputation:
- Read online reviews on Google, Yelp, or healthcare directories
- Ask for references from current or past clients
- Check for complaints or disciplinary actions with state regulatory boards
3. Evaluate Staff Qualifications and Training
The quality of the home health care team is critical. Consider:
- Education, licensing, and experience of nurses, therapists, and aides
- Ongoing training programs and professional development
- Background checks and screening procedures for all staff
4. Ask the Right Questions
When contacting agencies, ask detailed questions to ensure they can meet your needs:
- What services are provided, and how frequently?
- How are care plans developed and updated?
- How do they handle emergencies or changes in condition?
- Can they provide bilingual or culturally competent staff if needed?
- Are caregivers consistent, or will multiple caregivers rotate frequently?
5. Compare Costs and Insurance Coverage
Understanding cost structures and coverage is essential:
- Typical home health care costs vary depending on services and frequency of visits
- Medicare, Medicaid, and private insurance may cover certain services
- Ask about out-of-pocket expenses and financial assistance programs
Table: Typical Home Health Care Costs by Service Type
| Service Type | Average Cost (per visit/hour) | Notes |
|---|---|---|
| Skilled Nursing | $100–$200 | Varies with complexity of care |
| Physical/Occupational Therapy | $80–$150 | Typically 30–60 minutes per session |
| Home Health Aide | $25–$45 | Personal care and daily assistance |
| Chronic Disease Management Support | $60–$120 | Includes monitoring and education |
6. Assess Communication and Coordination
A strong agency maintains clear communication with:
- Patients and family members
- Doctors, therapists, and other healthcare providers
- Emergency services if needed
Agencies that prioritize communication ensure care is seamless, responsive, and safe.
Common Questions About Home Health Care
When considering home health care, families often have questions about safety, duration, services, and cost. Addressing these questions helps patients feel confident and ensures that care aligns with their needs.
1. Is Home Health Care Safe?
Yes, home health care is generally safe when provided by licensed and trained professionals. Safety measures include:
- Caregiver training in medical procedures and emergency response
- Background checks and screening for all staff
- Infection control protocols to reduce risk of illness
- Home safety assessments to prevent falls or accidents
Fact: According to the National Institute on Aging, patients receiving professional home health care experience fewer hospital-acquired infections than those in institutional settings.
2. How Long Can Someone Receive Home Health Care?
The duration of home health care varies depending on the patient’s needs:
- Short-term care: For post-surgery recovery or temporary illness, typically a few weeks to a few months
- Long-term care: For chronic conditions, disability, or aging in place, services can continue as needed with regular reassessment
Care plans are reviewed periodically to ensure that the patient receives appropriate support without unnecessary services.
3. How Often Do Caregivers Visit?
Frequency depends on the patient’s medical needs:
- Daily visits: Often for patients requiring skilled nursing or intensive therapy
- Several times per week: Common for therapy sessions or chronic condition monitoring
- Weekly or monthly visits: For stable patients needing light assistance or check-ins
Tip: Care plans are flexible and can be adjusted if a patient’s condition improves or worsens.
4. What Happens if a Patient’s Condition Worsens?
Home health care teams are trained to identify warning signs early. If a patient’s condition deteriorates:
- The nurse contacts the primary care physician immediately
- Care plans may be updated for more frequent visits or additional services
- Emergency services can be called if needed
This proactive approach helps prevent unnecessary hospitalizations and ensures timely intervention.
5. Can Home Health Care Be Short-Term or Long-Term?
Yes, home health care is highly flexible:
- Short-term: Ideal for recovery after surgery, illness, or injury
- Long-term: Supports chronic disease management, disability care, or aging in place
- Many agencies offer customized plans that adapt over time based on the patient’s progress
Tips for Families Managing Home Health Care
Managing home health care can feel overwhelming, especially for families balancing work, caregiving, and personal responsibilities. By following best practices, families can ensure that patients receive the highest quality care while maintaining safety and comfort at home.
1. Prepare Your Home for a Caregiver
A safe and organized home environment is crucial for effective home health care:
- Remove tripping hazards, such as loose rugs or cluttered walkways
- Ensure proper lighting in hallways, bathrooms, and staircases
- Install grab bars in bathrooms and handrails on stairs
- Arrange furniture to allow easy movement for patients using walkers or wheelchairs
- Keep essential items, medications, and emergency contacts easily accessible
2. Communicate Effectively with Care Providers
Clear communication with the home health care team ensures smooth coordination and reduces misunderstandings:
- Maintain a care journal documenting symptoms, medications, and daily activities
- Ask questions about changes in care plans, medications, or therapies
- Schedule regular meetings or calls with the primary nurse or care coordinator
- Share any concerns about the patient’s emotional or physical well-being
3. Monitor Health Changes
Families play a key role in observing subtle changes in the patient’s health:
- Watch for changes in appetite, sleep, or mood
- Report any new symptoms, pain, or difficulties with mobility
- Track vital signs like blood pressure, heart rate, or blood sugar if instructed by the care team
- Keep a record of medications, doses, and administration times
4. Support the Patient’s Independence
Encourage patients to do as much as they can safely manage:
- Allow them to perform tasks independently under supervision
- Provide adaptive equipment like walkers, reachers, or shower chairs
- Celebrate small achievements to boost confidence and morale
5. Take Care of Yourself as a Family Caregiver
Family members also need support to prevent burnout:
- Schedule breaks or respite care for yourself
- Seek guidance or training from home health professionals
- Join support groups for caregivers to share experiences and strategies
- Practice self-care and maintain a balance between caregiving and personal life
Quote: According to the Family Caregiver Alliance, “Caregivers who receive support and education are better able to provide safe, effective care and maintain their own well-being.”
Technology in Home Health Care
Technology is transforming home health care, making it safer, more efficient, and more accessible for patients and families. From remote monitoring to telehealth, modern tools enhance care quality while allowing patients to remain at home.
1. Remote Patient Monitoring Devices
Remote patient monitoring (RPM) allows caregivers and medical professionals to track vital signs and health metrics in real time:
- Devices can monitor blood pressure, heart rate, oxygen levels, blood glucose, and weight
- Data is automatically sent to the care team for review
- Alerts are triggered if readings indicate a potential problem, allowing early intervention
Example: A patient with congestive heart failure uses a wearable device that tracks weight and fluid retention. Alerts sent to the nurse prevent hospitalizations by identifying issues before they escalate.
2. Telehealth and Virtual Visits
Telehealth enables patients to connect with healthcare providers without leaving home:
- Video consultations with doctors, nurses, or therapists
- Remote assessments for chronic conditions, medication management, or therapy progress
- Reduces travel time and increases access to specialists, especially in rural areas
Fact: According to the American Telemedicine Association, telehealth in home care reduces hospital readmissions by up to 20% for chronic disease patients.
3. Mobile Apps for Health Management
Mobile apps support patients and caregivers in managing daily care:
- Medication reminders and tracking
- Symptom logging and reporting to the care team
- Scheduling of caregiver visits and therapy sessions
- Educational resources and instructional videos
Example: An app integrated with a home health agency allows a family to track the patient’s daily exercise routines, medication adherence, and vital signs in one platform.
4. Technology Improves Safety and Care Quality
- Fall detection sensors alert caregivers or emergency services immediately
- Smart home devices, like voice-activated assistants, help patients call for help or control home environments
- Data analytics allow agencies to monitor trends and proactively adjust care plans
Case Studies and Success Stories in Home Health Care
Real-life examples demonstrate how home health care can significantly improve recovery, independence, and quality of life for patients. These stories also illustrate the value of personalized care, skilled medical support, and family involvement.
Case Study 1: Post-Surgery Recovery at Home
Patient: 72-year-old female recovering from hip replacement surgery
Services Provided: Skilled nursing, physical therapy, and home health aide assistance
Outcome:
- Daily nursing visits for wound care and medication management prevented infections
- Physical therapy sessions helped the patient regain mobility faster than expected
- Home aide support ensured safe transfers and personal care
- Patient returned to independent living two weeks earlier than projected
Key Takeaway: Home health care allowed for faster recovery, fewer complications, and a safer environment compared to extended hospital stays.
Case Study 2: Chronic Disease Management
Patient: 68-year-old male with congestive heart failure and diabetes
Services Provided: Remote patient monitoring, nurse visits, medication management, dietary guidance
Outcome:
- Daily monitoring of weight, blood pressure, and blood sugar prevented acute episodes
- Coordinated care with the physician reduced emergency visits
- Patient maintained independence and quality of life while avoiding repeated hospitalizations
Fact: Studies indicate that patients with chronic conditions receiving home health care experience 30% fewer hospital readmissions.
Case Study 3: Support for a Patient with Stroke
Patient: 60-year-old female post-stroke
Services Provided: Physical therapy, occupational therapy, speech therapy, and caregiver support
Outcome:
- PT improved mobility and strength, OT assisted with daily tasks, and speech therapy enhanced communication
- Family training allowed caregivers to provide effective support at home
- Patient achieved greater independence in daily activities and regained confidence
Quote: “Home health care gave me the support I needed to recover in my own home, surrounded by my family. I felt safe, cared for, and motivated every step of the way.” – Patient testimonial
Key Insights from Success Stories
- Personalized care matters: Tailored plans improve outcomes and recovery times.
- Family involvement enhances care: Educated caregivers reinforce therapies and monitor health.
- Technology supports monitoring: Remote devices and apps prevent complications and alert caregivers promptly.
- Home environment promotes comfort: Familiar surroundings reduce stress and encourage healing.
Common Challenges in Home Health Care and How to Overcome Them
While home health care offers significant benefits, families and patients may encounter challenges. Being aware of these issues and proactive solutions ensures care remains effective, safe, and stress-free.
1. Staff Shortages and Scheduling Issues
Challenge: Some home health agencies face shortages of qualified nurses, aides, and therapists, leading to inconsistent care schedules.
Solution:
- Choose agencies with strong staffing policies and backup plans
- Confirm caregiver continuity so patients see familiar staff
- Ask agencies about emergency coverage and on-call support
2. Ensuring Quality and Consistency of Care
Challenge: Quality of care can vary depending on staff experience and agency protocols.
Solution:
- Verify staff credentials, training, and experience
- Request a detailed care plan and progress reports
- Communicate regularly with supervisors or care coordinators to monitor performance
3. Managing Multiple Caregivers
Challenge: Patients with complex needs may interact with several caregivers, which can cause confusion or inconsistencies.
Solution:
- Maintain a care journal to track daily activities, medications, and therapies
- Encourage clear communication between all caregivers
- Schedule regular check-ins with the care coordinator to align on patient needs
4. Safety Concerns and Fall Prevention
Challenge: Patients at home are at risk for falls or accidents, especially seniors or those with mobility issues.
Solution:
- Conduct a home safety assessment to identify hazards
- Install grab bars, handrails, non-slip mats, and adequate lighting
- Educate patients and families on safe mobility practices
- Consider wearable fall detection devices or emergency alert systems
5. Emotional and Psychological Challenges
Challenge: Patients may feel isolated or stressed by receiving care at home, and family caregivers can experience burnout.
Solution:
- Incorporate companionship and social support into care plans
- Offer respite care for family caregivers
- Utilize telehealth or virtual counseling for emotional support
The Future of Home Health Care
The demand for home health care is rapidly increasing due to an aging population, advances in medical technology, and a growing preference for receiving care at home. The future of in-home care promises more personalized, efficient, and technology-driven solutions for patients and families.
1. Trends in Aging Populations and Demand for In-Home Services
- The global population aged 65 and older is projected to double by 2050, increasing the need for home-based medical and personal care.
- Seniors prefer to “age in place,” making home health care a practical and preferred option over institutional care.
- Agencies are expanding services to meet the rising demand for chronic disease management, post-surgical care, and personal assistance.
2. Innovations in Medical Technology and Remote Care
Technology is transforming how home health care is delivered:
- Remote monitoring devices track vital signs and detect complications early
- Telehealth allows virtual consultations with doctors and therapists
- Wearable devices and smart home systems improve safety and independence
- Data analytics and AI help predict patient needs, optimize care plans, and reduce hospitalizations
Fact: According to a 2024 report by Grand View Research, the global home healthcare market is projected to reach $526 billion by 2030, driven by technology integration and growing demand.
3. Growing Role of Personalized Care Plans
- Future home health care will focus on highly individualized care, addressing medical, emotional, and social needs.
- Care plans will incorporate predictive analytics, patient preferences, and lifestyle factors to improve outcomes.
- Agencies are increasingly using interdisciplinary teams and digital tools to coordinate seamless care at home.
4. Integration with Broader Healthcare Systems
- Home health care will become more connected with hospitals, clinics, and insurance providers.
- Real-time data sharing allows for continuity of care, reducing readmissions and improving patient outcomes.
- Collaborative care models will ensure patients receive the right level of care at the right time.
Conclusion: Is Home Health Care Right for You?
Home health care offers a safe, effective, and personalized approach to medical and daily living support, allowing patients to receive professional care in the comfort of their own homes. From skilled nursing and therapy services to personal care and chronic disease management, home health care can meet the needs of seniors, post-surgical patients, individuals with chronic illnesses, and people with disabilities.
Why Consider Home Health Care
- Comfort and Familiarity: Patients remain in a familiar environment, which supports emotional well-being and faster recovery.
- Personalized Care: Individualized care plans ensure that medical, therapeutic, and daily needs are addressed effectively.
- Cost-Effectiveness: In-home care can be more affordable than extended hospital stays or long-term facility care.
- Family Involvement: Families can actively participate in care while receiving professional support and guidance.
- Technology and Innovation: Remote monitoring, telehealth, and smart devices enhance safety and efficiency.
Making the Decision
Families considering home health care should:
- Assess the patient’s medical and daily living needs
- Research reputable home health care agencies
- Discuss options with doctors and care coordinators
- Ensure services are covered by insurance or affordable
- Prepare the home for safe and comfortable care delivery
Call to Action: If you or a loved one need professional medical support while staying at home, explore licensed home health care agencies in your area. With the right team, tools, and planning, home health care can help patients recover faster, manage chronic conditions effectively, and maintain independence.