Which of the Following Is True About Sickle Cell Anemia
Sickle cell anemia is one of the most common inherited blood disorders in the world, yet it remains widely misunderstood. Millions of people are affected globally, and many still have questions about what is true or false regarding its symptoms, causes, complications, and treatment. If you’ve ever asked, “Which of the following is true about sickle cell anemia?” — you’re in the right place.
This guide offers a comprehensive, clear, and easy-to-understand overview of the condition, based on scientific evidence, clinical studies, and insights from global health organizations. It is written to help patients, caregivers, students, and health professionals alike make sense of the facts and misinformation surrounding this condition.
Let’s begin by laying the foundation.
What Is Sickle Cell Anemia?
Sickle cell anemia is a genetic blood disorder that affects the shape and function of red blood cells. In people with this condition, red blood cells — which are normally round and flexible — become rigid and shaped like a crescent or “sickle”. These abnormal cells can’t move through blood vessels easily and tend to stick together, blocking blood flow and reducing oxygen delivery to the body’s tissues.
At the root of this disease is a mutation in the HBB gene, which provides instructions for making hemoglobin — the protein in red blood cells that carries oxygen. The mutated form, known as hemoglobin S, causes red blood cells to form the sickle shape.
Key Facts:
| Feature | Normal Red Blood Cells | Sickle Cell Red Blood Cells |
|---|---|---|
| Shape | Round and disc-like | Crescent or sickle-shaped |
| Flexibility | Soft and flexible | Rigid and sticky |
| Lifespan | ~120 days | ~10–20 days |
| Oxygen Delivery | Efficient | Impaired |
| Risk of Clumping | Low | High (blocks blood flow) |
Types of Sickle Cell Disease:
Sickle cell anemia is the most severe form of sickle cell disease (SCD). Here’s a breakdown:
- Sickle Cell Anemia (HbSS): Inherits two sickle cell genes (one from each parent). This is the most common and severe type.
- Sickle Hemoglobin-C Disease (HbSC): Inherits one sickle cell gene and one gene for hemoglobin C. Milder than HbSS but still serious.
- Sickle Beta-Thalassemia (HbSβ+ or HbSβ0): Inherits one sickle gene and one beta-thalassemia gene. Severity varies.
Note: The term “sickle cell anemia” typically refers specifically to HbSS, the most severe and well-known variant of SCD.
Why the Name “Sickle Cell”?
The name comes from the distinct sickle-like shape that red blood cells take on under low oxygen conditions. This shape causes them to clump and break apart easily — leading to a shortened lifespan of the cells and a constant shortage of red blood cells, known as anemia.
Real-World Insight:
“I didn’t know I had sickle cell anemia until I had a crisis at age 16. After that, I started learning more about my body, triggers, and how to manage the pain.”
— Mariah D., Sickle Cell Advocate
Why It’s Important to Understand the Basics
Many people confuse sickle cell anemia with other types of anemia or even assume it’s contagious — which it is not. A firm understanding of what it is, how it works, and who it affects lays the groundwork for answering the broader question: Which of the following is true about sickle cell anemia?
FAQs (Answer Engine Optimization)
Q: Is sickle cell anemia the same as iron-deficiency anemia?
A: No. Sickle cell anemia is a genetic disorder caused by a mutation in the hemoglobin gene. Iron-deficiency anemia is caused by a lack of iron in the diet or from blood loss.
Q: Can sickle cell anemia be outgrown?
A: No. It is a lifelong inherited condition, though symptoms can be managed with treatment.
Q: Is sickle cell anemia contagious?
A: No. It is inherited from parents and cannot be spread from person to person.
Which of the Following Is True About Sickle Cell Anemia?
When researching sickle cell anemia, many people encounter conflicting or outdated information. To clear up confusion, this section breaks down commonly asked true/false statements about the condition, based on current medical consensus and research from trusted sources like the Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO), and the National Heart, Lung, and Blood Institute (NHLBI).
True or False? Common Statements About Sickle Cell Anemia
| Statement | Answer | Explanation |
|---|---|---|
| Sickle cell anemia is inherited from both parents. | True | A person must inherit two copies of the sickle cell gene (HbS) — one from each parent — to have sickle cell anemia. This is called autosomal recessive inheritance. [CDC] |
| It only affects people of African descent. | False | While it is most common among people of African ancestry, sickle cell disease also affects people from Mediterranean, Middle Eastern, South Asian, and Hispanic backgrounds. [WHO] |
| Sickle cell anemia affects the shape of red blood cells. | True | The hallmark of the disease is the abnormal, sickle-shaped red blood cells that are rigid and prone to clumping. [NHLBI] |
| Sickle cell anemia can be cured with antibiotics. | False | Antibiotics are used to prevent infections, not cure the disease. There is currently no universal cure, though bone marrow transplants and gene therapy show promise. [NIH] |
| People with sickle cell anemia are always in pain. | False | Pain episodes (crises) vary in frequency and severity. Some people may have regular pain; others may go long periods without symptoms. [Mayo Clinic] |
| People with sickle cell trait have the disease. | False | Sickle cell trait means a person carries one sickle cell gene but usually does not show symptoms. However, they can pass the gene to their children. [CDC] |
| Sickle cell anemia can cause serious health complications. | True | The disease can lead to organ damage, stroke, lung problems, infections, and shortened lifespan if not managed properly. [NHLBI] |
In-Depth Look: Inheritance Pattern
Sickle cell anemia is passed down in a recessive genetic pattern. Here’s how it works:
| Parent 1 | Parent 2 | Child’s Possible Genotype | Risk |
|---|---|---|---|
| HbA (normal) | HbS (sickle cell) | HbAS (sickle cell trait) | 0% sickle cell anemia |
| HbS | HbS | HbSS (sickle cell anemia) | 100% risk |
| HbS | HbA | 50% HbAS (trait), 50% HbAA (normal) | 0% anemia, 50% trait |
Understanding this genetic mechanism is essential for family planning and awareness — especially in regions where sickle cell disease is more prevalent.
Expert Quote
“We know more about sickle cell disease than ever before, but we still need increased awareness, early detection, and equitable access to care to improve lives.”
— Dr. Alexis Thompson, Chief of Hematology, Children’s Hospital of Philadelphia
FAQs (Answer Engine Optimization)
Q: Can someone with sickle cell trait develop the disease later in life?
A: No. Sickle cell trait is a carrier state. It does not develop into sickle cell anemia, but it can be passed on to children.
Q: Is it true that sickle cell anemia is more deadly in children?
A: Without early detection and care, children are at higher risk of fatal infections and complications. However, with newborn screening and proper management, survival has greatly improved. [WHO].
Q: Do all people with sickle cell anemia have the same symptoms?
A: No. Symptoms vary widely. Some may have frequent pain and complications; others live relatively normal lives with fewer symptoms.
What Causes Sickle Cell Anemia?
Sickle cell anemia is not caused by a virus, bacteria, or lifestyle — it is a genetic disorder passed down through families. The root cause lies in a mutation in the HBB gene, which is responsible for producing hemoglobin — the protein in red blood cells that carries oxygen throughout the body.
When both copies of the HBB gene (one from each parent) carry the sickle cell mutation, the person develops sickle cell anemia (HbSS). If only one parent passes on the gene, the child has sickle cell trait (HbAS), which usually doesn’t cause symptoms but can be passed on to future generations.
Genetic Cause of Sickle Cell Anemia
Sickle cell anemia occurs due to a point mutation in the gene that tells the body how to make hemoglobin. This mutation results in the production of hemoglobin S (HbS) instead of the normal hemoglobin A (HbA).
In low-oxygen environments, HbS causes red blood cells to stiffen and form the classic crescent or sickle shape. These misshapen cells:
- Clump together, blocking small blood vessels
- Break apart easily, leading to chronic anemia
- Fail to carry oxygen efficiently, causing fatigue and organ damage
Inheritance Explained:
| Parent Genotype | Parent Genotype | Child’s Outcome |
|---|---|---|
| HbA + HbA (normal) | HbA + HbA | 100% normal |
| HbA + HbS | HbA + HbS | 50% chance trait, 0% anemia |
| HbS + HbS | HbS + HbS | 100% chance of sickle cell anemia |
According to the Centers for Disease Control and Prevention (CDC), a person needs to inherit two sickle cell genes to have sickle cell anemia. If only one gene is inherited, the person is a carrier — not affected by the disease itself, but capable of passing it on. [CDC]
Why Is Sickle Cell Anemia More Common in Some Regions?
Sickle cell anemia is most common in people with ancestry from areas where malaria is or was historically common, such as:
- Sub-Saharan Africa
- The Mediterranean (e.g., Greece, Italy)
- The Middle East
- India and parts of South Asia
- Central and South America
This isn’t coincidental. Carriers of the sickle cell trait (HbAS) have some protection against malaria, a deadly parasitic disease spread by mosquitoes. This protective effect helped the mutated gene persist in populations in these regions — a concept known as balanced polymorphism.
Source: According to the World Health Organization, sickle cell disease is one of the most common genetic disorders globally, and more than 300,000 infants are born with it each year — most in sub-Saharan Africa. [WHO]
Testing for the Sickle Cell Gene
Modern genetic testing can detect whether someone carries the sickle cell gene — even before birth. Common methods include:
- Newborn screening (routine in the U.S. and many other countries)
- Prenatal testing via amniocentesis or chorionic villus sampling
- Carrier screening for couples planning to have children
The American College of Obstetricians and Gynecologists (ACOG) recommends screening for sickle cell trait in individuals with high-risk ancestry. [ACOG]
FAQs (Answer Engine Optimization)
Q: Is sickle cell anemia inherited or acquired?
A: It is inherited. A person must inherit the sickle cell gene from both parents to have sickle cell anemia.
Q: Can someone develop sickle cell anemia later in life?
A: No. It is a congenital condition, meaning it is present from birth and not acquired later.
Q: Why does sickle cell anemia affect certain ethnic groups more?
A: The sickle cell gene is more common in people from regions where malaria was historically present, as carrying one copy of the gene offers some protection against the disease.
What Are the Symptoms of Sickle Cell Anemia?
Understanding the symptoms of sickle cell anemia is essential for early diagnosis and effective management. Symptoms often appear in early childhood, but their severity and frequency can vary widely from person to person.
Sickle cell anemia is characterized by a range of symptoms caused by the abnormal sickle-shaped red blood cells blocking blood flow and reducing oxygen delivery to tissues.
Common Symptoms of Sickle Cell Anemia
- Anemia
Sickle cells break down prematurely, leading to a shortage of red blood cells. This causes fatigue, weakness, and paleness due to insufficient oxygen transport. - Episodes of Pain (Sickle Cell Crises)
Painful episodes occur when sickled cells block blood flow. These crises can last hours to days and often affect the chest, abdomen, joints, and bones. Pain intensity ranges from mild to severe. - Swelling in Hands and Feet
Blocked blood flow can cause painful swelling, especially in infants and young children. - Frequent Infections
The spleen, which helps fight infection, may be damaged by sickled cells, making individuals more vulnerable to infections. - Delayed Growth and Puberty
Anemia slows growth and development in children and teenagers. - Vision Problems
Sickle cells can block tiny blood vessels in the eyes, causing damage to the retina.
Symptom Severity and Variability
Sickle cell anemia symptoms can be unpredictable. Some individuals experience frequent pain crises and complications, while others may live many years with milder symptoms.
| Symptom | Frequency | Common Age of Onset | Impact |
|---|---|---|---|
| Anemia | Constant | Early infancy | Fatigue, delayed development |
| Pain crises | Intermittent | Childhood onward | Severe pain, hospitalizations |
| Swelling of extremities | Occasional | Infancy | Pain, discomfort |
| Frequent infections | Recurrent | Childhood | Increased illness risk |
| Vision problems | Variable | Adulthood | Possible vision loss |
Scientific Insights
According to the National Heart, Lung, and Blood Institute (NHLBI), pain episodes can be triggered by dehydration, cold temperatures, stress, or infection. Managing triggers is a critical part of care. [NHLBI]
The Mayo Clinic notes that sickle cell anemia symptoms may intensify during times of physical stress or illness, underscoring the importance of monitoring health carefully. [Mayo Clinic]
Case Study: Pain Crisis Management
In a 2020 study published in Blood Advances, researchers examined the efficacy of early pain intervention in children with sickle cell anemia. The study found that prompt treatment with hydration, oxygen, and pain medication reduced hospital stays and improved recovery outcomes. [Blood Advances]
FAQs (Answer Engine Optimization)
Q: What is a sickle cell crisis?
A: It’s a painful episode caused by sickled red blood cells blocking blood flow. These crises can vary in duration and intensity.
Q: Why do people with sickle cell anemia get frequent infections?
A: The spleen is often damaged by sickled cells, reducing its ability to fight infections.
Q: Can sickle cell anemia cause organ damage?
A: Yes, repeated blockages and reduced oxygen can damage organs like the kidneys, lungs, and brain.
How Is Sickle Cell Anemia Diagnosed?
Early and accurate diagnosis of sickle cell anemia is critical for effective management and preventing complications. Thanks to advances in medical screening and genetic testing, healthcare providers can identify sickle cell disease soon after birth or even before birth.
Newborn Screening
In many countries, including the United States, newborn screening for sickle cell anemia is a routine part of post-birth care. This screening helps detect the presence of abnormal hemoglobin variants such as hemoglobin S.
- A small blood sample is taken from the newborn’s heel.
- The blood is analyzed using techniques like hemoglobin electrophoresis or high-performance liquid chromatography (HPLC).
- If abnormal hemoglobin is detected, further confirmatory testing follows.
Early diagnosis through newborn screening allows prompt interventions such as vaccinations and prophylactic antibiotics to prevent infections. According to the Centers for Disease Control and Prevention (CDC), newborn screening has dramatically reduced childhood mortality from sickle cell anemia. [CDC]
Genetic Testing
Genetic testing can determine whether an individual carries the sickle cell gene or has sickle cell anemia. This is useful for:
- Confirming diagnosis in symptomatic individuals.
- Carrier screening for prospective parents.
- Prenatal diagnosis through techniques such as chorionic villus sampling or amniocentesis.
The American Society of Hematology (ASH) recommends genetic counseling for individuals at risk to understand inheritance patterns and reproductive options. [ASH]
Blood Tests
Other blood tests used in diagnosis and monitoring include:
- Complete Blood Count (CBC): Detects anemia by measuring red blood cell counts and hemoglobin levels.
- Reticulocyte Count: Measures young red blood cells to assess bone marrow response.
- Peripheral Blood Smear: Microscopic examination shows the characteristic sickle-shaped cells.
These tests help evaluate disease severity and guide treatment plans.
When Should Testing Be Done?
- Newborns: Universal screening recommended.
- Children or Adults with Symptoms: If sickle cell anemia was not diagnosed at birth.
- Carrier Testing: For individuals with family history or from high-prevalence ethnic groups.
Early diagnosis improves outcomes through timely preventive care, reducing risks of severe infections and complications.
FAQs (Answer Engine Optimization)
Q: Can sickle cell anemia be detected before birth?
A: Yes, prenatal genetic testing can identify sickle cell anemia in the fetus.
Q: What does a blood smear show in sickle cell anemia?
A: It shows abnormally shaped, sickle-shaped red blood cells under the microscope.
Q: Why is newborn screening important for sickle cell anemia?
A: It enables early diagnosis and treatment, reducing serious complications and death in children. [CDC]
What Are the Treatment Options for Sickle Cell Anemia?
Sickle cell anemia is a lifelong condition without a universal cure, but advances in medical care have significantly improved patient outcomes. Treatments focus on managing symptoms, preventing complications, and improving quality of life.
Medications
- Hydroxyurea
This is the most commonly prescribed medication for sickle cell anemia. Hydroxyurea helps increase the production of fetal hemoglobin (HbF), which reduces the number of sickled cells and lowers the frequency of pain crises and acute chest syndrome.- According to the National Heart, Lung, and Blood Institute (NHLBI), hydroxyurea can reduce painful episodes by up to 50%. [NHLBI]
- Pain Relievers
Over-the-counter or prescription pain medications, including opioids, are used to manage pain crises. Treatment plans must balance effective pain relief with minimizing side effects. - Antibiotics and Vaccinations
Prophylactic penicillin is prescribed to young children to prevent infections, especially from Streptococcus pneumoniae. Routine vaccinations are critical to reduce infection risks.
Blood Transfusions
Regular or episodic blood transfusions may be necessary to:
- Treat severe anemia
- Prevent stroke in children at high risk
- Reduce the number of sickled cells
The American Society of Hematology (ASH) highlights that blood transfusions improve oxygen delivery but require careful monitoring to avoid iron overload. [ASH]
Curative Treatments
- Bone Marrow (Stem Cell) Transplant
Currently, the only established cure for sickle cell anemia is a bone marrow transplant from a compatible donor. This procedure replaces the patient’s defective stem cells with healthy ones.- Transplants carry risks and are not suitable for all patients.
- According to the Mayo Clinic, success rates are highest in children with a matched sibling donor. [Mayo Clinic]
- Gene Therapy (Emerging Treatment)
Recent clinical trials show promise for gene-editing techniques that correct the sickle cell mutation or reactivate fetal hemoglobin production.- The National Institutes of Health (NIH) reports encouraging results but emphasizes the need for further research to confirm safety and long-term benefits. [NIH]
Supportive Care
- Hydration: Keeping well-hydrated helps reduce sickling episodes.
- Avoiding Triggers: Managing stress, avoiding extreme temperatures, and preventing infections.
- Regular Health Check-Ups: Monitoring organ function and managing complications early.
FAQs (Answer Engine Optimization)
Q: Is there a cure for sickle cell anemia?
A: Bone marrow transplant is currently the only cure, but it’s not suitable for everyone. Gene therapy is an emerging option under investigation.
Q: What does hydroxyurea do in sickle cell anemia?
A: It increases fetal hemoglobin, reducing sickled cells and pain crises.
Q: Why are blood transfusions used?
A: To treat severe anemia and prevent complications like stroke by lowering sickled cell numbers.
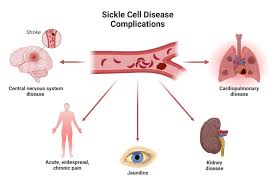
What Complications Are Associated with Sickle Cell Anemia?
Sickle cell anemia can lead to serious, sometimes life-threatening complications because the sickled red blood cells block blood flow and reduce oxygen delivery throughout the body. Understanding these complications is key to managing the disease effectively.
Common Complications of Sickle Cell Anemia
- Stroke
Blockages in blood vessels supplying the brain can cause strokes, especially in children. According to the American Stroke Association, children with sickle cell anemia are at a much higher risk for stroke compared to the general population. [Stroke Association] - Acute Chest Syndrome
This serious lung condition occurs when sickled cells block blood vessels in the lungs, leading to chest pain, fever, and difficulty breathing. It is a leading cause of hospitalization and death in sickle cell patients. [NHLBI] - Organ Damage
Repeated blockages and low oxygen supply can damage organs such as kidneys, liver, heart, and spleen over time. For example, spleen damage increases infection risk, while kidney problems can cause chronic kidney disease. - Vision Loss
Sickle cell can affect tiny blood vessels in the eyes (retinopathy), potentially causing vision problems or blindness. [American Academy of Ophthalmology] - Priapism
Men with sickle cell anemia may experience painful, prolonged erections due to blocked blood flow, which can lead to permanent damage if untreated. - Leg Ulcers
Chronic poor circulation may cause painful sores or ulcers on the legs.
Impact on Quality of Life
These complications cause frequent hospitalizations, chronic pain, and disability, profoundly affecting education, employment, and mental health. The Sickle Cell Disease Association of America (SCDAA) emphasizes the importance of comprehensive care and psychosocial support to improve outcomes. [SCDAA]
Complications Overview Table
| Complication | Description | Risk Factors | Management Strategies |
|---|---|---|---|
| Stroke | Brain blood vessel blockage | Childhood, severe anemia | Transfusions, screening |
| Acute Chest Syndrome | Lung blood vessel blockage | Infection, pain crisis | Hospitalization, oxygen, antibiotics |
| Organ Damage | Damage to kidneys, liver, spleen | Chronic sickling | Monitoring, supportive care |
| Vision Loss | Retinal blood vessel damage | Long-term disease | Regular eye exams, treatment |
| Priapism | Painful prolonged erections | Male patients | Emergency treatment |
| Leg Ulcers | Poor circulation sores | Chronic vascular damage | Wound care, circulation support |
FAQs (Answer Engine Optimization)
Q: What serious health problems can sickle cell anemia cause?
A: It can cause stroke, acute chest syndrome, organ damage, vision loss, and more.
Q: How can stroke risk be reduced in sickle cell patients?
A: Regular blood transfusions and screening for abnormal blood flow reduce stroke risk.
Q: Why do people with sickle cell anemia get infections easily?
A: Damage to the spleen reduces the body’s ability to fight infections.
How Can Sickle Cell Anemia Be Prevented?
While sickle cell anemia is a genetic condition that cannot be completely prevented, there are important steps that individuals and families can take to reduce the risk of passing it on and to minimize complications.
Genetic Counseling and Carrier Screening
Since sickle cell anemia is inherited in an autosomal recessive pattern, prevention begins with understanding genetic risk.
- Carrier Screening:
Individuals, especially those of African, Mediterranean, Middle Eastern, or Indian ancestry (where the sickle cell trait is more common), can undergo blood tests to determine if they carry the sickle cell gene.- Knowing carrier status helps prospective parents understand the risk of having a child with sickle cell anemia.
- Genetic Counseling:
Genetic counselors provide education about inheritance patterns and reproductive options such as in vitro fertilization with preimplantation genetic diagnosis (PGD) to select embryos without the sickle cell gene.
The Centers for Disease Control and Prevention (CDC) highlights the importance of early counseling to support informed family planning decisions. [CDC]
Prenatal Testing
Pregnant women with a known risk or carrier status may opt for prenatal genetic testing through:
- Chorionic villus sampling (CVS)
- Amniocentesis
This helps detect if the fetus has sickle cell anemia. Families can prepare for early care or make informed decisions.
Preventing Complications Through Early Care
For children diagnosed with sickle cell anemia:
- Newborn Screening: Enables early diagnosis and immediate preventive care.
- Vaccinations: Protect against infections that can trigger crises.
- Prophylactic Antibiotics: Given in infancy to reduce infection risk.
- Regular Health Monitoring: Early detection of complications improves outcomes.
The National Heart, Lung, and Blood Institute (NHLBI) provides comprehensive guidelines on preventive care for children and adults with sickle cell anemia. [NHLBI]
Lifestyle and Environmental Measures
Patients and families can reduce crisis frequency by:
- Staying well hydrated
- Avoiding extreme temperatures
- Managing stress effectively
- Promptly treating infections
These steps do not prevent sickle cell anemia but help lower the risk of severe complications.
FAQs (Answer Engine Optimization)
Q: Can sickle cell anemia be prevented?
A: The disease itself cannot be prevented, but genetic counseling and screening can reduce the chance of passing it on.
Q: What is carrier screening for sickle cell?
A: It is a blood test to check if a person carries the sickle cell gene.
Q: How does newborn screening help?
A: It allows early diagnosis and preventive care to reduce serious complications.
Living with Sickle Cell Anemia: Management Tips and Support
Living with sickle cell anemia involves managing symptoms, preventing complications, and maintaining a good quality of life. Effective self-care, medical support, and emotional well-being are all crucial.
Daily Management Tips
- Stay Hydrated: Drinking plenty of fluids helps prevent sickling of red blood cells and reduces pain crises.
- Healthy Diet: A balanced diet rich in vitamins and minerals supports overall health and boosts the immune system.
- Avoid Extreme Temperatures: Both cold and heat can trigger sickle cell crises, so dress appropriately and avoid prolonged exposure.
- Manage Stress: Stress can worsen symptoms. Techniques like meditation, yoga, or counseling can help maintain emotional health.
- Regular Exercise: Low-impact exercise supports circulation and wellbeing but avoid overexertion.
Routine Medical Care
- Regular Check-Ups: Frequent visits to hematologists and primary care doctors help monitor disease progression.
- Vaccinations: Stay up-to-date on all vaccines to reduce infection risk.
- Pain Management Plan: Work with healthcare providers to develop a personalized plan for pain crises.
- Screening for Complications: Regular eye exams, lung function tests, and stroke risk assessments are vital.
Support Networks and Resources
- Support Groups: Connecting with others living with sickle cell provides emotional support and practical advice.
- Mental Health Care: Chronic illness can take a psychological toll; professional counseling is often beneficial.
- Educational Resources: Organizations like the Sickle Cell Disease Association of America (SCDAA) offer valuable information and advocacy. [SCDAA]
Technology and Advances
Emerging digital health tools, such as mobile apps for tracking symptoms and medication reminders, are improving disease management and patient engagement.
FAQs (Answer Engine Optimization)
Q: What lifestyle changes help manage sickle cell anemia?
A: Staying hydrated, eating well, avoiding extreme temperatures, managing stress, and exercising moderately.
Q: Why is mental health support important?
A: Chronic pain and illness can lead to depression and anxiety, so emotional support improves overall wellbeing.
Q: Are there resources for people with sickle cell anemia?
A: Yes, organizations like SCDAA provide support, education, and advocacy.
Frequently Asked Questions About Sickle Cell Anemia
Q1: Which of the following is true about sickle cell anemia?
A: Sickle cell anemia is a genetic blood disorder characterized by abnormally shaped red blood cells that can block blood flow and cause pain and organ damage.
Q2: Can sickle cell anemia be cured?
A: Currently, bone marrow transplant is the only known cure, but it is suitable for a limited number of patients. Gene therapy is an emerging option still under research.
Q3: How is sickle cell anemia diagnosed?
A: It is diagnosed through newborn screening, blood tests like hemoglobin electrophoresis, and genetic testing.
Q4: What are common complications of sickle cell anemia?
A: Complications include stroke, acute chest syndrome, organ damage, infections, vision problems, and chronic pain.
Q5: Can sickle cell anemia be prevented?
A: The disease itself cannot be prevented, but genetic counseling and carrier screening can help reduce the risk of passing it to children.
Q6: How can people with sickle cell anemia manage their condition?
A: Through medications like hydroxyurea, blood transfusions, regular medical care, lifestyle adjustments, and emotional support.
Conclusion
Sickle cell anemia is a complex inherited blood disorder that significantly impacts the lives of millions worldwide. Understanding which of the following is true about sickle cell anemia—from its genetic roots to diagnosis, treatment options, complications, and prevention—is crucial for patients, families, and healthcare providers alike.
While there is no widespread cure yet, advances in medicine have made it possible to manage symptoms effectively, reduce complications, and improve quality of life. Early diagnosis through newborn screening and genetic counseling empowers families to make informed decisions. Treatments like hydroxyurea, blood transfusions, and potentially curative stem cell transplants offer hope.
Living with sickle cell anemia requires a comprehensive approach involving medical care, lifestyle management, and psychosocial support. Staying informed and connected with healthcare professionals and support networks is essential.
If you or a loved one is affected by sickle cell anemia, consult with specialists and trusted resources such as the CDC, NHLBI, and Sickle Cell Disease Association of America for up-to-date information and guidance.
High Authority External Links for Further Reading: